Diving Safety
The Causes, Physiology, and Process of Drowning
Globally, nearly 40 people die from drowning every hour of every day, and though seldom the trigger, it is the number one cause of diver fatalities. Even so, drowning is poorly understood by the diving public, and surprisingly, by many professionals who investigate drowning incidents. Here diving instructor trainer and medicolegal death investigator Andrea Zaferes, who has spent more than 30 years investigating aquatic deaths and teaching water rescue/recovery with her partner, Butch Hendrick of Lifeguard Systems, explains what divers need to know about drowning.

by Andrea Zaferes, Copyright Forensic Aquatic Consulting & Training LLC 2021
Header Image by Derk Remmers. Other Figures and images courtesy of LifeGuard Systems unless noted.
In general, drowning is an outcome of unsafe events or medical emergencies occurring in aquatic environments. Nearly 40 people die from drowning every hour worldwide. There are about ten drowning fatalities daily in the U.S. where drowning is the number one most common cause of accidental death to children aged one through four years. Drowning is also the most common cause of diver fatalities.1 Despite its tragically high prevalence, drowning is often poorly understood by the general population and also by a large percentage of professionals who work in aquatic industries, who investigate drowning events (i.e. law enforcement, death investigators), first responders, and sometimes medical personnel.
My experience working with thousands of sport divers, dive leaders, public safety divers, and military divers worldwide during the last 36 years has taught me that too few divers fully understand specifically what drowning is, the underlying physiological processes, the implications for those who survive it, and most importantly, the many different precipitating events.
Drowning is a process that is usually initiated by a chain of events that could have been prevented with more thorough academic knowledge, better decision-making, and more effective, evidence-based hands-on training.
A poor understanding of drowning has consequences that range from missing prevention and rescue opportunities, missing early signs and symptoms, less than optimal rescue and first aid, denial or misinterpretation of delayed physiological and psychological consequences of drowning, as well as a surprisingly large number of homicides incorrectly diagnosed as accidents, suicides, or a natural disease process.
Drowning is a diagnosis of exclusion, meaning it should be the diagnosis that is left over after all other possible differential diagnoses are ruled out. There are no universally accepted medical tests to conclusively prove a person drowned, other than perhaps diatom testing which is plagued by confusion and misinformation, is not well used in the U.S., and is beyond the scope of this article. That drowning is a diagnosis of exclusion is an important issue for the diving community, as no doubt some drowning fatalities have been incorrectly diagnosed as drowning accidents when they were cardiac-related natural deaths, while others misdiagnosed as cardiac natural deaths were actually drowning accidents that then were complicated by cardiac problems. Accurately determining the cause of death, and the manner of death一i.e., natural, accidental, suicide, homicide, or undetermined一is critical for diver safety and justice.
If a death is ruled a natural death due to cardiomyopathy一or chronic heart disease一the most common conclusions are that the death would have occurred anywhere; that it was not the fault of a diver, dive leaders, the dive training agency, or the dive industry; and likely couldn’t have been prevented aside from better medical screening. On the other hand, the death of a diver with cardiomyopathy who receives inadequate or even negligent dive training, and drowns as a complication of cardiac problems that were precipitated by unnecessary physical and mental stress and negligently inadequate skills, is an accident. In that case, the dive industry bears some responsibility.
Too few medical examiners or coroners who determine cause and manner of diver deaths have sufficient training and experience regarding dive incident investigation to work these cases without a multidisciplinary team including a diving expert, law enforcement, and a diving physician to accurately determine diving fatality cause and manner of death for all diving fatalities.
As divers, our understanding of drowning causes, processes, pathophysiology, and outcomes can make a difference. We can help prevent drowning, understand and perform important aspects of rescue techniques and first aid, recognize early and delayed signs and symptoms, and help effectively document critical incident information that can facilitate correct cause and manner of death determinations.
What is drowning?
Attendees of the 2002 World Drowning Congress in Amsterdam, Nederland, came to a consensus in adopting the following definition:
“Drowning is the process of experiencing respiratory impairment from submersion/immersion in liquid.”2
This definition lacks an important aspect, namely “airway submersion/immersion in liquid with liquid aspiration.”
Layon etl al. (2009) state, “Implicit in this definition is that a liquid/air interface is present at the entrance of the victim’s airway, preventing the victim from breathing air.”3 I prefer a definition without implications, and I believe that liquid aspiration is a necessary component of drowning that should be presented in the definition.
This is especially true because there are non-drowning causes of respiration impairment from submersion/immersion that might not include airway submersion/immersion. Divers, as potential victims of respiration impairments, should be aware of their lethal potential.
Swimming-induced pulmonary edema, also known as immersion pulmonary edema (IPE), is an example of how immersion can result in potentially lethal respiratory impairment without water aspiration. “Swimming-induced pulmonary edema occurs when fluid accumulates in the lungs in the absence of water aspiration during swimming and produces acute shortness of breath and a cough with blood-tinged sputum.”4

A diver’s respiration can also be impaired during cold shock from sudden immersion in cold water. This respiratory impairment can involve initial uncontrolled gasps and hyperventilation. A third example of how immersion can result in respiratory impairment without drowning is immersion hypothermia48, which can result in a slowing of respiration leading to hypercapnia and hypoxia.5
The Center for Disease Control and Prevention uses the following definition for drowning in the definitions for non-injury fatalities: “Suffocation (asphyxia) resulting from submersion in water or another liquid.”6 Dr. Craig Nelson, a forensic pathologist and NAUI instructor offers a nice, clear, simple definition: “Asphyxia due to airway submersion in a liquid.”
I propose the following definition of drowning: “Drowning is fatal or nonfatal asphyxia from airway immersion in liquid with liquid aspiration.” The reason I feel the last three words are necessary is because there are still some holdouts who believe that a person can drown without actually inhaling any liquid into the lungs. “Fatal” and “nonfatal” is important because victims who survive and initially feel fine after possible aspiration need to realize that they may have experienced drowning and must be monitored for the development of possible delayed signs and symptoms of morbidity for the next several days.
Those definitions beg the question: What is asphyxia? Asphyxiation is a process that directly causes oxygen deprivation. There are several types of asphyxiation such as drowning, confined space suffocation, and strangulation.7 Asphyxia is the resulting state of oxygen deprivation. Thus, drowning and strangulation can directly result in the state of asphyxia.
Another way of classifying drowning as a form of asphyxiation is to view water as a hazardous atmosphere. The National Fire Protection Agency defines hazardous atmosphere as that which does not sustain life. Without the personal protection equipment of a scuba regulator or surface supply hard hat, airway submersion can result in death in about four to six minutes.
Other drowning terms most heard by divers, such as “dry drowning,” “wet drowning,” “near-drowning,” and “secondary drowning” are not supported by evidence, perpetuate myths, and add unnecessary confusion to a diagnosis of drowning. Today there is only one term: drowning.

The Drowning Process
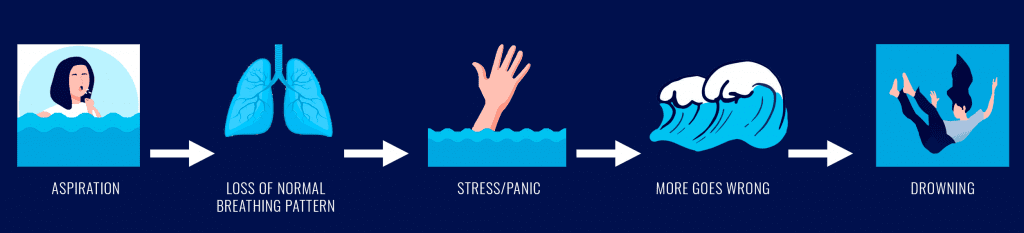
Aspiration can cause the initiation of the drowning process. For example: A poorly trained diver’s mask floods and water enters the nasal passages. The diver aspirates a small volume of water, begins coughing, normal breathing patterns are lost, the diver panics, rips his mask off, spits his regulator out, and bolts to the surface. During the ascent there could be a breath hold, but eventually the diver starts aspirating and the drowning process progresses.
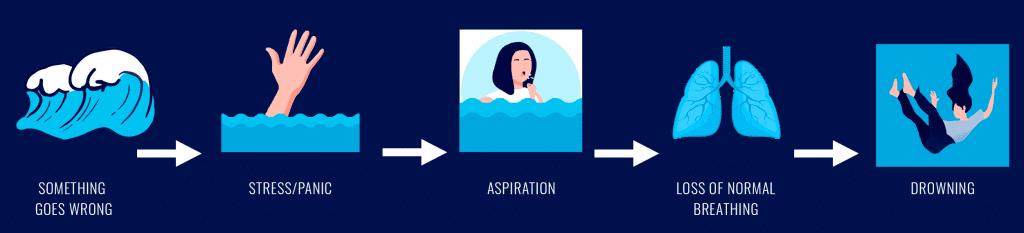
In other cases, something goes wrong in the water, struggling victims can no longer keep their airways dry, and aspiration occurs with loss of normal breathing, initiating the drowning process. In these cases, it is believed that the most common sequence of events includes:
- Voluntary breath-hold when the airway is immersed or submerged.
- Elevation of the respiratory waste product carbon dioxide in the arterial blood (hypercarbia), signals the brain to initiate breathing.
- The victim can no longer maintain the breath hold, and water enters the oral/nasal passages.
Once fluid enters the nose or mouth there are three places it can go. In order from best to worst options, the fluid can be spit or snorted out of the body. If it enters the pharynx, the start of the throat, it can be swallowed, or worse, it can progress down into the larynx that functions as a valve on top of the trachea.8
Fluids entering the nasopharynx and oropharynx can progress into two different tubes. The less damaging option is the fluid’s entry into the esophagus, the tube located posteriorly to the trachea, where it is swallowed into the stomach. That would be swallowing, not aspiration. It is suggested that drowning victims swallow significantly larger volumes of water than they inhale, which increases the chances of vomiting spontaneously or during resuscitation.9 Vomiting could increase the later risk of aspiration pneumonia if the drowning victim survives more than a day or two.
If, on the other hand, the fluid travels more anteriorly, it can reach the epiglottis that serves as a trap door that closes to keep food and fluid out of the larynx when eating or drinking. Fluid that enters the larynx can then descend into the trachea. To help prevent that, the respiratory system has what could be called a defense mechanism called a laryngospasm. Think of it as an involuntary breath hold. Breath hold means no oxygen getting in or carbon dioxide getting out. This could result in hypercapnia and possibly hypoxia. Hypercapnia can result in increased respiratory effort that could continue to be obstructed if the laryngospasm continues. It is believed that swallowing fluid down the esophagus into the stomach could ensue.
If a laryngospasm does not occur, or when it releases, then fluid can enter the trachea, the left and right main bronchi, and down through the smaller airways until it reaches the microscopic air sacs called alveoli. Now the pathophysiology can become more severe and complicated.
Drowning Pathophysiology
Once we start talking about what happens inside the body during the drowning process, we begin the discussion of drowning pathophysiology— the abnormal functions or disordered physiological processes that are the result of disease, injury, or a syndrome. Knowledge about the pathophysiology of the drowning process, which begins with inhalation of fluid, can help us better recognize early signs and symptoms, and take the most effective pre-hospital course of actions.
If a diver breathing from a snorkel at the surface instead of a regulator begins struggling against a current to reach a boat, inhales water, and has a severe coughing fit, that diver should be medically evaluated and monitored for later complications associated with nonfatal drowning. The diver might refuse medical evaluation because of embarrassment or lack of symptoms. If dive leaders or other persons present have an understanding of the potential pathophysiology, they could explain the possible fatal consequences of not being evaluated to help convince the diver to agree.
Knowledge of pathophysiology is also important to increase the effectiveness of rescue procedures and prehospital and hospital medical care. If in-water rescuers can envision the ill effects of inhaled fluid washing away the surfactant coating the alveoli in the victim’s lungs, perhaps they will make greater efforts to protect airways from further fluid entry as they transport victims to land or boats.
An understanding of the presentation and causes of the pulmonary edema that might appear to be literally pouring out of an unresponsive drowning victim’s airway can help first responders understand that they can, and should, ventilate the victim directly through the pulmonary edema and not waste time attempting to suction it away. Knowledge can help paramedics understand that, for patients with acute pulmonary edema, frequent endotracheal tube suctioning might not be recommended “because it creates a negative alveolar pressure, harming already damaged capillaries and entraining more oedema fluid.”10

Effective treatment of pulmonary complications in drowning depends on the lung pathophysiology that occurred during and after aspiration, as well as the bacteria or other contaminants involved in the aspiration. As Bierens et al (2002) explain in their paper, “Understanding the pathophysiology of drowning may help us to understand lung injuries and ischemic brain injuries.”11
The Role of Alveoli: A basic introduction to alveoli physiology will aid an understanding of how inhaled fluid can damage alveoli. Bronchial airways connect to alveolar ducts that terminate in alveolar sacs. The alveolar region makes up approximately 90% of lung tissue.12 Effective and sufficient gas transfer (oxygen in and carbon dioxide out) requires a large surface area consisting of a thin barrier through which gas can be transferred and diffused. In the lungs, the interalveolar septum is that barrier. It separates the alveolar air compartment from the blood in the pulmonary capillaries embedded in it, and in its totality consists of a large, thin surface area.
Alveoli must be capable of withstanding being stretched when inspired gas volumes are large, and need stability to not collapse when volumes are low. Connective tissue in between the interalveolar septum serves to prevent alveolar overdistension. Surfactant protects alveoli from collapsing inward.
Pulmonary surfactant, a mixture of approximately 90% lipids and 10% proteins,13 forms a surface film inside alveoli14 and is critically necessary for the pulmonary and gas exchange steps in the process of respiration. Surfactant was part of the evolutionary process allowing species to move from water to air breathing.15 Without pulmonary surfactant, which reduces the surface tension of water, we would not have effective gas exchange16 and our alveoli would collapse (atelectasis).17 Surfactant also helps keep fluid from pulmonary capillary blood from leaking into the alveoli, reduces respiratory effort, and even is part of the immune system.18
Pulmonary edema: Pulmonary edema can be a significant part of the drowning process for both fatal and nonfatal cases. There are two types of pulmonary edema: cardiogenic and noncardiogenic. Cardiogenic pulmonary edema can arise when blood pools or increases in pressure on the left side of the heart, which backs up the oxygenated, “clean” blood attempting to travel from the lungs to the left side of the heart where it is pumped throughout the body. Conditions that can cause this include congestive heart failure (CHF), cardiomyopathy, left side heart valve disease, some cardiac arrhythmias, and heart attacks that result in left ventricular failure.
It is possible that immersion and other stresses of diving are risk factors for exacerbating such problems as CHF that could trigger respiratory issues during a dive that could then lead to drowning. For example, hydrotherapy has not been recommended for patients with CHF because immersion can cause an increased venous return and increase in ventricular filling pressure.19 It would be challenging to accurately distinguish between drowning or complications of CHF as the initiating factor for such a dive incident be it fatal or nonfatal. Such a determination would require a thorough and expert review of the circumstances of the dive.
Drowning involves the latter that is caused by “direct injury/damage to lung parenchyma/vasculature.”20 That direct injury is caused by fluid entering the parenchyma. Drowning victims are believed to inhale approximately 3-4 ml/kg of body weight, so it does not take a large volume of water in the lungs to initiate the drowning process. Lunetta et al. (2004) reviewed 578 autopsies of persons who “presumably” drowned, and found that 98.6% of them presented with pulmonary edema.21
Pulmonary edema is therefore a nonspecific finding—its presence does not tell you its causes, which are many, including opioid overdoses, the cardiac problems listed above, over-hydration prior to immersion, immersion pulmonary edema, high altitude sickness, sepsis, acute respiratory distress syndrome (ARDS), toxin inhalation, advanced kidney disease, brain trauma, aspirin OD, pulmonary embolism, and tonic-clonic seizures. Pulmonary edema, by itself, cannot be used to diagnose drowning. Circumstances and other medical findings, or lack thereof, must be investigated and considered.
When fluid enters the alveoli during the drowning process, it damages the surfactant, which is called “surfactant washout.” This surfactant destruction decreases gas diffusion, allows fluid from the blood to enter the alveoli which worsens the edema problem, and can result in alveoli collapse (atelectasis). This means that the levels of oxygen in the blood decrease (hypoxemia) and levels of carbon dioxide can increase (hypercapnia). If the blood has too little oxygen, then so will the body’s tissues, including heart and brain parenchyma (“the functional tissue of an organ as distinguished from the connective and supporting tissue”22) resulting in a state of hypoxia.
Additionally, pulmonary edema can result in hypercapnia that can upset the body’s delicate pH balance causing acidotic changes. These changes can result in cardiac dysfunction and arrest and central nervous system ischemia (inadequate blood supply). When those two critical organs fail, then anoxia can result in death—i.e., fatal drowning. Pulmonary edema can cause additional damage to alveoli. Alveoli containing fluid have been shown in rat models to affect the interalveolar septum associated with neighboring gas filled alveoli and causing over-expansion in the latter.23
As discussed, it does not take a large volume of inhaled water to cause fatal drowning. Are there consequences of greater volume inhalations? The literature suggests that a fluid aspiration of at least 11 ml/kg is necessary for blood volume changes, and more than 22 ml/kg is required for significant changes in blood electrolytes.24 25
As for the question of differences between fresh and saltwater drowning pathophysiology, contemporary research and literature find insufficient evidence to support a difference between drowning mediums.26 Such findings can be present with both salt and freshwater drownings.
Drowning pathophysiology includes additional complications in nonfatal drowning, including “decreased lung compliance, ventilation-perfusion mismatching, and intrapulmonary shunting, leading to hypoxemia that causes diffuse organ dysfunction”27 28, that are beyond the scope of this article.
Drowning outcome terminology and pathology
The updated consensus on terms for the possible outcomes of drowning are “death,” “morbidity,” and “no morbidity.” Morbidity is operationally defined in this article as a state of disease, or more broadly, ill health.29 Morbidity can include physiological as well as mental ill health.
Van Beeck et al. (2005) raised the important issue that, “It is important to understand that drowning is not always fatal and nor is the obvious need for medical treatment.” Hence, “fatal” and “nonfatal” are other commonly used outcome terms today. The problem with only having a two-outcome system as compared to a system with three levels (fatal, nonfatal, nonfatal with morbidity) is that “nonfatal” does not differentiate between patients who have no residual ill health from the drowning event and those who do.
This becomes of particular importance when considering the impact of nonfatal cases, which are sometimes also referred to as “near misses,” that do have morbidities.
Consider a diver who survived inhaling 20 ml/0.68 fl oz of seawater while panicking after his mask was accidentally kicked off during a night dive. He appeared fine on shore, said he was fine, and was allowed to go home alone without a medical evaluation and without someone checking on him during the night. The danger is that he could develop pulmonary edema during the night resulting in fatal cardiac arrest while he was in bed. And, should that not happen, he could possibly end up with pneumonia.
One challenge to consider is that it may not always be clear if a drowning survivor has residual effects immediately after a nonfatal drowning event. An understanding of the drowning process could help us recognize the possibility that a person may have experienced a nonfatal drowning and alert all involved of the need for medical evaluation and monitoring.
How often does nonfatal morbidity or death occur after potential drowning events? The fatality rate appears to be decreasing in the U.S. “The death rate in 1970 was 3.87 deaths per 100,000 population, in 1980 it was 2.67, in 1990 it was 1.6, and in 2000 it was 1.24 deaths per 100,000 population.”30 This decline is possibly due to the improvement of rescue resources, prehospital medical care, and medical treatment rather than a decline in the number of drowning events. What would be useful is to compare the number of nonfatal to fatal drowning rates each decade.
The temperature of the water and the presence of contaminants can also affect patient outcomes. Colder water is associated with greater chances of long-term survival and survival with fewer neurological sequelae (conditions that are consequences of a prior disease or injury). Contaminants in the water can increase the chances of infections and complications.
Drowning victims who survive for one or more days could develop nonfatal or fatal respiratory illnesses and complications such as pneumonia, acute respiratory distress syndrome (ARDS), and hypoxic-ischemic brain injuries with cerebral edema, and increased intracranial pressures. Survivors can have long-lasting or permanent neurological and cognitive deficits.
Why do divers drown?
For drowning to occur, one or more of the following three factors must be present to initiate the chain of events that leads to inhalation of fluid:
- Insufficient skill level
- Incapacitation
- Insufficient, faulty, or missing personal protective equipment
Precipitating events include dive mask flooding, being caught in strong currents, feeling chest pain, falling into extremely cold water, poor diver gas management (i.e. running out of gas), unexpected zero visibility, diver overweighting, being told to meet a dive leader on the bottom when the bottom is unexpectedly well below the planned depth, being lost by an inattentive or poorly trained dive leader, entanglement, entrapment, inhaling water when hit in the face with a wave, poor buoyancy control, equipment failure, and pre-existing health problems.
Sometimes factors #2 and #3 can be the precipitating event itself. Triathlon swimmers might become incapacitated by immersion pulmonary edema to the point of a fatal drowning. Divers experiencing severe chest pains from angina could easily panic, spit out their regulator, and rip off their masks as they unsuccessfully struggle to reach the surface.
Lippman et al. (2013) lists rough water, buoyancy control, equipment problems as the most common causes of asphyxiation diver fatalities. Drowning is the main cause of diver asphyxiation death. Consider rough water. At some point water can become so rough that there is no amount of skill level that can make it safe in which to dive. The skill level then implies having the knowledge-based skill to be able to evaluate the water and make the correct determination to say “no” to the dive. Rough water can also cause incapacitation;for example, surge could push a diver inside a wreck and into rope entanglements, or bang a diver’s head on a wreck or a buddy’s tank.
Incorrect equipment can interact with rough water to increase the risk of incapacitation. For example, split fins and hinge fins do not provide wearers with as much power to move against currents as other fins. Divers wearing the former could have a decreased ability to prevent diver incapacitation or exertion when faced with current or surge pushing them into high-risk locations or situations than divers wearing fins that allow strong kicks to have more power and control in rough water.
Buoyancy control falls into the skill level category. Poor buoyancy control can also be compounded by incorrectly used equipment such as when divers are over-weighted and/or when their buoyancy compensating device’s (BCD) power inflator hoses are not connected properly—both of which have occured in a frightening number of recent diver fatalities during classes.31

Insufficient skill level
If PPE is not worn to keep divers afloat, then they need a certain degree of watermanship skills in order to stay on the surface because, except for infants and toddlers whose fat-to-muscle/bone ratio is greater, almost all humans are negatively buoyant. Fat floats, muscle sinks.
Some might be saying, “But wait, I float in water, so I need a few pounds of lead in order to descend even if I’m wearing only a bathing suit.” However, many who think they need weight without an exposure suit most likely don’t; but, more importantly, the reason some can easily stay on the surface with little to no effort is because they have air in their lungs. Every pint of air is equivalent to approximately 0.5 kg/1 lb of buoyancy.32
Consider this example using Archimedes’ principle:
dry weight – displacement weight = wet weight
Using 1kg/L (64 lb/ft3) for seawater,33 suppose the dry weight (on land) of a body is 91.6 kg/202 lb. The body displaces 92.1 kg/203 lb of seawater (90.6 L/3.2 ft3). That body will float with a positive buoyancy of 0.45 kg/1 lb. One pound of that body will be above the surface of the water and 91.1 kg 201 lb will be below the surface.
What occurs if 1.9 L/4 pints of air escape from the body? As every pint of air is equivalent to approximately 0.45 kg/1 lb of buoyancy, the body will have lost 1.8 kg/4 lb of upward force. Since the weight of air is negligible—4 pints of air weigh 0.01 lb 34—there is no real change in the downward force of the body’s mass—its weight on land. Therefore, once the 1.9 L/4 pints of air leave the body, the body will have a net weight of 1.4 kg/3 lb negative buoyancy in seawater. The body will sink to the bottom if no obstructions catch it on the way down.
Some people don’t need to exhale in order to sink; their fat to muscle ratio is so low that, even with 5.7 L/12 pints of air in their lungs, they will still sink. The rest have to release some of that gaseous buoyancy in order to become denser than the surrounding fluid medium.
As we drown, air escapes from our lungs, and we lose that buoyancy, pint for pint, liter for liter. Drowning victims do not sink, as some people think, because of water entering the lungs. If water enters lungs without air escaping, that will do little to change buoyancy because water weighs the same inside of the body as it does outside of the body. The added dry weight of 0.95 L/2 pints of water will be offset by an increased displacement volume of the body. If you add 2 pints of water to your drysuit when fully submerged without letting any air escape, it will not change your buoyancy.
Walt Butch Hendrick, founder of TeamLGS35, demonstrated this in a film he made for a drysuit manufacturer who was being sued for a diver drowning fatality. The plaintiffs opined that the drysuit valve failed, allowing water to enter the suit, causing the diver to become so negatively buoyant that he drowned. In the film, Hendrick dons a drysuit and scuba gear, descends to 30 m/100 ft, and makes himself neutrally buoyant with his BCD with no air in the drysuit. He then unzips the drysuit and fills it with water. The result is that he remains neutrally buoyant. The added upward force (displacement volume weight) of the added water was equal to the added downward force of the weight of the water inside the suit. He then makes a slow, effortless, and neutrally buoyant ascent to the surface. The drysuit valve leakage did not cause the diver to fatally drown.
Does saltwater make a difference since it is denser than freshwater? We are slightly more buoyant in salt water than in freshwater, but a large portion of drownings occur in saltwater environments.
Specific gravity: The key to whether or not a person sinks is specific gravity. Specific gravity is a term used to reference relative density. It is “the ratio of the density of a given material at a given temperature to the density of an equal volume of water at the same temperature.”36 The specific gravity of a substance is almost the same as its density in g/cm3. The substance’s density g/cm3 ÷ 1 g/cm3 = substance density = specific gravity.37
Specific Gravity = Psubstance / Preference
The most common reference substance is water at 3.98° C/39.2° F when water is at its densest state of 1 g/cc. Hence, at approximately 4o C/39.2° F, the specific gravity of fresh water is 1, which is convenient as water is the most common fluid involved in aquatic death investigation. Specific gravity is therefore a dimensionless number. Water at temperatures greater than 3.98° C/39.2° F will decrease in density as temperature increases. Freshwater at 10° C/50° F has a specific gravity of 0.988, and is 0.958 at 37.8° C/100° F.39 Water at colder temperatures is also less dense than water at 3.98° C/39.2° F—remember that ice floats.
Divers who make beach entries in white water waves need to be aware that, in addition to water movement issues, there are also specific gravity issues that can increase the risk of drowning should they lose their regulators from their mouths. Seawater is denser than freshwater, but surface water in areas where waves break could have lower specific gravities than freshwater. White water contains air bubbles that significantly lower its specific gravity to the point that diver airways can sink below the foam even with fully inflated BCDs.
If a person has a specific gravity greater than 1, the person will sink in 4o C/39° F freshwater. Values for healthy males between 20 and 40 years of age fall between 1.021-1.097.40 Females tend to have a slightly lower specific gravity. The primary determinant of human body specific gravity is the amount of adipose or fat tissue.
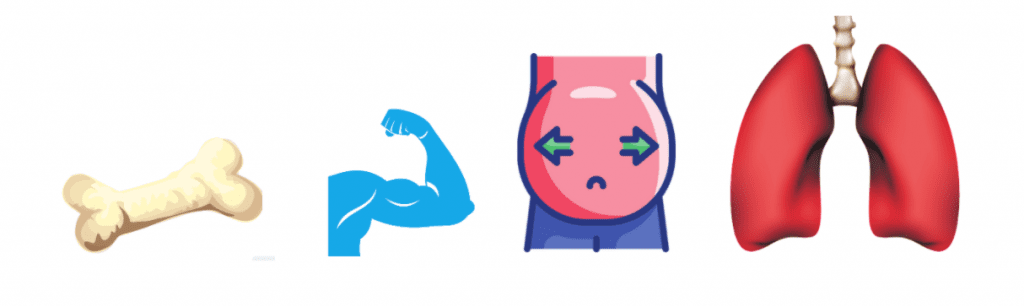
The density of adipose tissue (fat) is 0.9196 g/ml, 41 1.06 g/ml for mammalian muscle tissue,42 43 and 1.85 g/ml for bone.44 The density of fresh water is approximately 1 g/ml. Fat, being less dense than water, will float, and muscle and bone, being denser than water, will sink. It is therefore useful to know a person’s body type when considering the buoyancy and surface survival time of that particular individual.
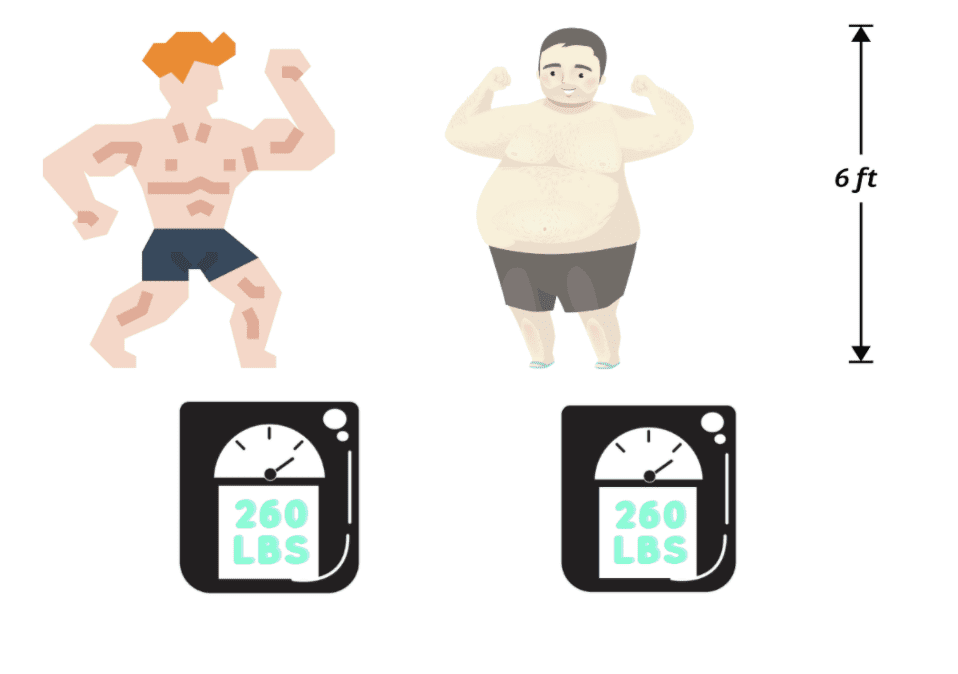
For an individual to have a specific gravity of less than 1, namely for an individual to be less dense than freshwater at 4o C/39° F, the percentage of body fat needs to be at least 61.7%. This shows that bodies sink in freshwater unless they are morbidly obese. The specific gravity of seawater is approximately 1.028, so a similar conclusion can be made for immersion in ocean water.

A competition body builder, therefore, may have a significantly shorter survival time on the surface than a friend with equal swim skills who has enough body fat to float comfortably with lungs half full of air. The body builder will sink even when lungs are fully expanded with air once he is too exhausted to keep himself at the surface with the use of his arms and legs. An additional survival variable not related to buoyancy is that the body builder has less insulation than the friend with more body fat and may experience the effects of cold stress—such as muscle fatigue and cramping— more quickly than his more insulated swim buddy.
Lung tissue has an even lower specific gravity than does adipose (fat) tissue and certainly has the greatest variability than any of our tissues since its specific gravity changes dramatically depending on the amount of gas in our alveoli (microscopic air sacs where gas exchange takes place). The issue of lung density which directly affects the buoyancy of lung tissue is complicated. For example, the blood content of lungs can change the density of lung tissue, and something as simple as body position (recumbent versus vertical) can change blood content and therefore can affect lung tissue density.
Weight belts: When weight belts were the mainstay of carrying weights, it was very possible to train divers how to reflexively ditch their weights at the first possibility that drowning was a possibility, and it was equally possible to train dive leaders how to ditch the weights of divers-in-need to prevent drowning. Such is no longer the case.

Today, divers are faced with a plethora of weight ditching mechanisms found in the wide variety of weight systems ranging from traditional weight belts, a plethora of weight-integrated BCDs, and several weight harness systems. Many tech divers dive without removable weights.
A study in Australia by DAN Asia found that 92% of diving fatality victims were found wearing their weight belts—in the days when almost all divers wore weight belts.45 That’s pretty frightening, since the majority of those divers were dying from drowning. If they had ditched their weights, most of them would have been positively buoyant on the surface and many would have survived rather than died. We weren’t training divers well enough to develop muscle memory, let alone reflexivity, in regard to that lifesaving skill of ditching weights to stay alive—that was when we all wore weight belts.
Now divers are buying and renting weight integrated BCDs with little or no training to ditch the weights in the myriad of different weight systems being used today. Pull out, pull down, grab the little tab, pull the T-bar, grab the handle, use one hand, need both hands… And think about dive leaders who are often faced with two, three, or more different weight systems within each group they lead or teach. Muscle memory? Reflexivity? How?

Now that we understand that we need skills or positively buoyant PPE to keep our airways above the surface of the water, let us consider variables associated with skill levels.
All divers, by standard, should have a degree of swim skills such as being able to perform a continuous 61 m/200 yd swim without touching bottom. So why is drowning the most common cause of diver fatality? Most of the dive incident near-misses and drowning fatalities that my partner/mentor Walt Butch Hendrick and I have studied had insufficient skills as the main cause of the incident.
These include negligently poor dive leader skills, weak kicking skills, overweighting, insufficient training in breathing underwater with a flooded or no mask, weak underwater movement skills (e.g. using hands), and lack of understanding of personal limitations.
Incapacitation
Incapacitation is “the state of not having the necessary ability, qualification, or strength to perform some specified act or function.”46 In regard to drowning, the specified act is keeping one’s airways dry such that air—not water—is inhaled. Except for cases of suicide, people who purposefully enter water intend on eventually coming out alive.
What causes incapacitation to the point of drowning? That question is the first step in the most important discussion regarding drowning—how to prevent it. In order to drown in water that is shallow enough to easily stand up in, something has to cause victims to become incapacitated enough such that they can no longer keep their airways sufficiently above the drowning medium. Law enforcement, medical examiners, and coroners who did not fully understand this seemingly simple concept have incorrectly determined a number of body-found-in bathtub homicides to be drowning accidents or suicides.
Anytime people are found dead in water shallow enough to maintain their airways, we must find the cause of what incapacitated them—what prevented them from keeping their airways dry. If no incapacitating factors are discovered after an effective investigation, then the risk of the manner of death being homicide is significantly increased.
It is important to understand that people with some swimming skills can drown in water slightly shallower than their airway height if they are so panicked that they do not realize that they can stand up. Sometimes incapacitation is caused by inadequate skills.
If you have been active in the dive industry long enough, in the last 15-20 years—when the overall skill levels of new divers have noticeably decreased—you likely have observed divers flailing in shallow water when trying to change from a horizontal to vertical position because they lack the basic skill of turning 180 degrees to a supine (face-up) position while tucking their finned-feet under them prior to standing up. Such divers, if overweighted, can panic and sink below the surface, possibly losing or spitting out their regulator.
People who have fallen through ice-covered water have drowned in water shallow enough to stand up in when cold shock47—or eventually, immersion hypothermia48—caused cardiac arrhythmias49 or muscle incapacitation when they were not rescued in time.
The U.S. Coast Guard has software that predicts the range of time that a person wearing a lifejacket can survive with consideration of such variables as water temperature, water movement, air temperature, and the person’s height and weight. Such persons might become incapacitated by fatigue, since the way most lifejackets fit requires a degree of effort to keep the wearer from falling into a prone (face-down) position into the water. Immersion hypothermia can decrease their survival time, as can being continuously splashed in the face by waves.
There are a number of incapacitating events to consider when investigating drowning incidents, developing rescue procedures, or developing drowning prevention policies.
Medical incapacitation: Cardiovascular events, diabetic emergencies, ruptured aneurysms, and seizures can incapacitate even strong swimmers to the point of drowning. Caruso (2006) found that 130 out of 877 (approximately 15% of) diving fatalities from 1990-1999 in the U.S. were attributed to cardiovascular disease. Lippman (2013) examined 351 diver fatalities from 1972-2005, and found that 19% were cardiac related. Those instances are increasing over time, most likely due to the aging diving population. The industry appears to be failing at bringing in and keeping younger divers, which is a topic that could fill a series of articles.
Medical issues raise the point that bodies recovered from water do not always involve drowning as a cause of death. As stated above, drowning is a diagnosis of exclusion. This means that a diagnosis of drowning is made when the circumstances involve airway submersion and there is no other obvious cause of death. Autopsy findings might include significant atherosclerotic heart disease and signs of long-term, uncontrolled hypertension, making cardiac arrhythmia50 a possible cause of death.
An additional complication is how to determine if the arrhythmia caused incapacitation and drowning, or if death was so sudden that it occurred before the drowning process could start. And, perhaps the drowning process itself caused an already diseased heart to have fatal arrhythmias as the drowning process progressed to hypoxemia. Was cause of death drowning alone, cardiac arrhythmias alone, or a combination? If the latter, which was the precipitating mechanism? That question might be unanswerable.
Why do we care? We should care because if drowning was the sole cause of death, or the precipitating mechanism, then we have to ask how skill level, incapacitation, or poor PPE were responsible for the death and how we can prevent such future deaths. If the death was strictly due to a medical event, then changing diving variables might not be the answer to preventative measures.
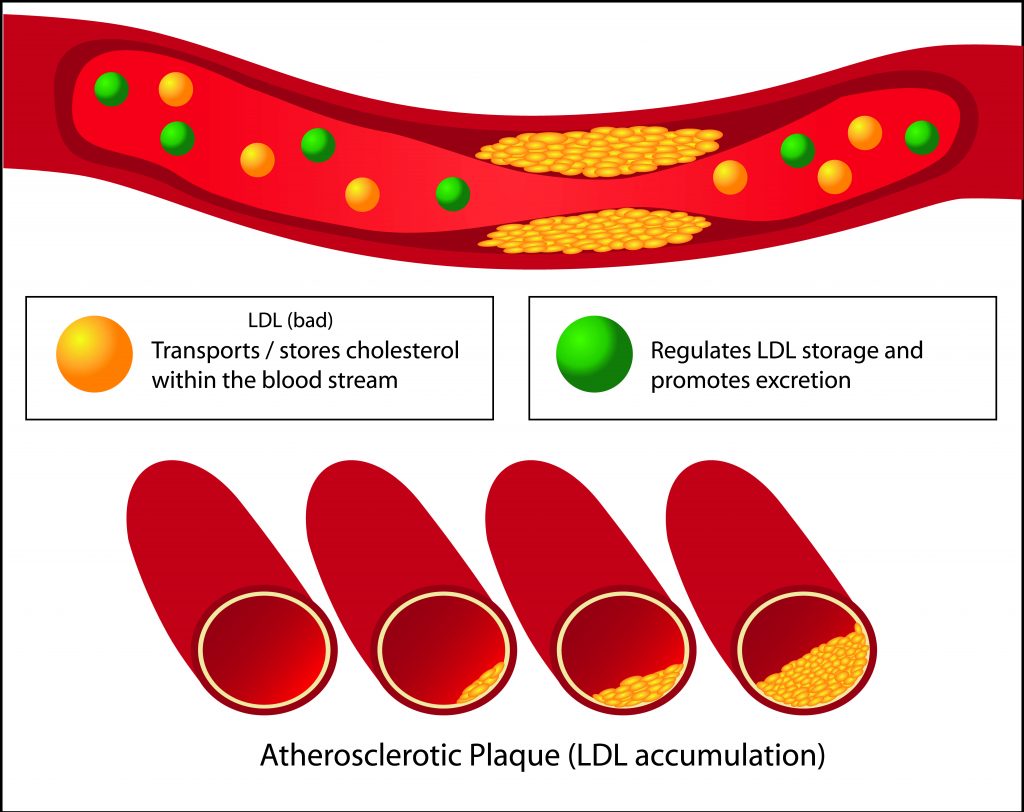
Cardiac dysrhythmias, or heart rhythm problems, themselves do not present signs during autopsies, so they too are often a diagnosis of exclusion. In older individuals, there are cardiac pathologies that are associated with arrhythmias. Atherosclerotic coronary artery disease with uncontrolled hypertension and advanced age, for example, are used in arrhythmia cause of death diagnosis-of-exclusion determinations. In young descendants who lack such medical histories, diagnosing a cardiac arrhythmia cause of death can be challenging.51 There are a series of cardiac disorders that can cause sudden unexpected death in young people, but the findings can be equivocal and may require extensive family medical history investigations and specialized, expensive tests that may not be in the budget of a medical examiner or coroner office budget.
Thus, in diving fatalities it is imperative that true experts in diving fatality investigations must be consulted before drowning or a sudden arrhythmic death syndrome causes of death determinations are made. If the former, we need to look at possible weak diving skills, inadequate dive training, poor decision-making, or dive leader negligence. If the latter, then neither the dive industry, a dive leader, or the diver may be at fault.
Was the drowning due to incapacitation from a natural disease process interacting with the water environment, such as an asthma attack stimulated by cold water aspiration or poorly controlled diabetes in conjunction with strenuous and long duration kicking? Or, perhaps, did the diver drown because she had a myocardial infarction—i.e. heart attack—while underwater that was exacerbated by the mental and physical stress of trying to keep up with the rest of the divers who were equally working hard to keep up with a too-fast swimming dive leader?
Panic: Consider what the state of panic is and how it can incapacitate someone to the point of drowning. Panic is defined as “sudden uncontrollable fear or anxiety, often causing wildly unthinking behavior.”52 Panic is a sudden sensation of fear, which is so strong as to dominate or prevent reason and logical thinking, replacing it with overwhelming feelings of anxiety and frantic agitation consistent with an animalistic fight-or-flight reaction. Panic may occur singularly in individuals or manifest suddenly in large groups as mass panic (closely related to herd behavior).”53
The late Dr. Lee Somers described a Caribbean case history to the author for which he served as an expert witness. Dive leaders negligently dropped a group of divers off in water with a depth below 46 m/150 ft, telling them to meet the dive leaders on the bottom. As divers sank to the bottom, panic ensued resulting in multiple fatalities. A fingernail of one female diver was found embedded in the neck of a dead divemaster.

Panicked divers have been known to spit out regulators, rip off masks, make uncontrolled ascents, and physically refuse regulators from would-be rescuers not trained to manage that problem. The advent of relatively inexpensive underwater video cameras has provided the dive industry with the ability to closely observe post-incident the missed signs of impending problems that led to outright panic and, very sadly, sometimes fatal diver drownings. We all need to study these tragic videos to learn what went wrong and how we as an industry can work together to fix the sometimes all-too obvious problems.
Neurological impairments: Seizures and diving don’t mix well as, sadly, some divers experiencing oxygen toxicity have demonstrated. The author had the experience of spending a surprisingly long duration communicating with a teen and his father who had a hard time understanding why the author removed the teen from a resort course when he suddenly appeared to have lost consciousness near the bottom of a 5.5 m/18 ft tank. The pair didn’t see why it was necessary to write “narcolepsy” under “other” in the teen’s medical liability waiver.
Technical divers, particularly rebreather divers, face increased risk of losing consciousness due to oxygen toxicity, hypoxia, or hypercapnia as a result of an inappropriate breathing mix in their loop, which could result in drowning in the absence of a mouthpiece retaining strap (MRS) and or effective rescue.
When alcohol or illicit drug intoxication plays a part in drowning deaths, intoxication can be included as a contributory cause of death on death certificates. In diving, nitrogen narcosis can similarly cause mental impairment in divers54 that could be attributed to drowning and other causes of death, such as pulmonary barotrauma if an uncontrolled ascent occurs. Unfortunately, nitrogen narcosis cannot be diagnosed with autopsy or toxicology findings. Its importance as a contributing factor to diving injury or death can be equally important as a contributing factor such as alcohol intoxication and, hence, signs of its presence should be investigated and considered.

Cold water: Incapacitation leading to drowning can involve only a few muscles in the body. Divers with inadequate, faulty, or a complete lack of gloves in cold water can experience significant loss of hand dexterity.55 Take a moment to think of one or two ways you could drown while diving if your hands become nonfunctional. And then, when in doubt, always wear the warmer of your gloves.
There are a number of other categories of incapacitating factors that have not been presented in this article. Consider sitting down with a group of your fellow divers and discuss and create a list of others. The Diver Medic and Team Lifeguard Systems Facebook pages post drowning case histories that can be used in meaningful drowning recognition and prevention discussion. If you have case histories to share—whether they be near-misses, nonfatal drownings, or fatal drownings—post them so others can learn from them.
Faulty, incorrectly used/worn, or missing personal protective equipment (PPE)
Unlike 50 years ago, contemporary diving equipment presents few failures when properly maintained and used. So, the issue today is more often incorrectly-worn or over-used equipment.
Too much lead put in diver weight systems is one of the most common forms of incorrectly used personal protective gear (PPE) and has been a major factor in a series of diver fatalities. Not having BCD power inflators properly connected is another issue that the author is seeing with greater frequency. Using a drysuit instead of the BCD to maintain neutral buoyancy is another potentially dangerous practice as too much air in a drysuit can result in more serious problems than too much air in a BCD. The use of aluminum, standard pressure tanks with backmounted BCDs that were designed for heavy, high-pressure, multiple steel tanks can increase the chances of drowning on the surface.
In January 2021, the Rebreather Training Council (RTC) launched a new rebreather safety initiative designed to prevent drowning in the event of a rebreather diver losing consciousness underwater. Specifically, the RTC now recommends the use of an MRS when diving a rebreather. It further recommends that rebreather divers be taught about the advantages of an MRS during their training, and that vendors supply them with their rebreathers (as is required according to the European rebreather standard EN14143).

It is widely acknowledged that the use of rebreathers increases the probability of exposure to an inappropriate breathing gas, which can lead to a Loss of Consciousness (LoC). As sport rebreather diving community leaders, the RTC and its members believe the specific risk of water aspiration following LoC underwater must be proactively mitigated. An MRS is an easy-to-use, easy-to-fit device that prevents the mouthpiece from being lost in the event of LoC, and can therefore minimize the risk of immediate drowning.
Understanding the causes
Drowning is designated in a number of studies as one of the principal causes of diver fatalities.56 57 The results from such epidemiology studies regarding cause of death should be considered with the following caveat. Many, if not most, autopsies performed on divers are standard autopsies as opposed to diver-specific autopsies performed by forensic pathologists with an expertise in diving death investigation and who understand the importance of multidisciplinary58 investigations. It is important to evaluate the process by which cause of death was determined for diving fatalities before using cause of death determinations in research, legal actions, and policy changes.
And, when making a determination that drowning was the cause of death, for any reason, it’s important to note that drowning does not necessarily explain what caused a fatality. When drowning is the final cause of death diagnosis, it is still critical to determine what caused the drowning. Did a healthy diver become incapacitated on the surface while exerting themselves in a current with the exertion being exacerbated by over-weighting, a poor kicking technique, and a lack of self-rescue skills, with the final result that the diver unwillingly submerged without a regulator in their mouth? Did the diver drown after incurring an incapacitating arterial gas embolism during a rapid, uncontrolled ascent initiated by a flooded mask and ensuing panic?
There is also the question of manner of death (accidental, natural, suicide, homicide, or undetermined). If a diver has a sole cause of death being a cardiac arrhythmia secondary to cardiac disease with no evidence of drowning, then a reasonable manner of death is natural. If the cause of death involves drowning, pulmonary barotrauma, or decompression sickness, then the death will likely be considered accidental, but not always.
Perhaps the drowning of an elderly man was caused by a suicide. He spent his savings on a trip where he appeared to purposefully drown himself while free-diving in waters off what he thought was the most beautiful place in the world.60 Or, did a diver drown when his father purposefully turned off his air with the intent to kill the diver, as tragically occurred during a recreational quarry dive in Canada?61
Each of those incidents might have listed drowning as cause of death, but the events leading up to the cause were markedly different in each case. In the first two cases, training and perhaps skill maintenance were the initiating problems, and in the third case perhaps poor medical history screening and early sign/symptom recognition were at least in part to blame.
In Conclusion
Drowning is the most common cause of death for divers. Despite 40 people drowning hourly worldwide, drowning is often poorly understood. It is a diagnosis of exclusion, meaning that diagnosis is left over after all other possible differential diagnoses have been ruled out, and it is frequently misdiagnosed by professionals who work in aquatic industries. Unfortunately, knowing that a diver drowned does not necessarily explain what caused the fatality.
In this article, we explained what drowning is and described the drowning process and its pathophysiology including the consequences of inhaling water such as surfactant washout and accompanying pulmonary edema. We also identified the three possible outcomes of drowning being fatal, nonfatal, and nonfatal with morbidities.
We then discussed the factors that must be present to initiate the chain of events leading to the inhalation of fluid, these being insufficient skill level; incapacitation; and insufficient, faulty, or missing personal protective equipment. We hope that this information will help you to better understand the nature of drowning so that you can avoid it and render effective assistance to others in the event of an incident. Safe diving.
Footnotes:
1 Wikipedia: Scuba diving fatalities
2 Van Beeck EF, Branche CM, Szpilman D, Model JH, Bierens JJLM. A new definition of drowning: towards documentation and prevention of a global public health problem. Bull World Health Organ. 2005;83:853-856.
3 A Joseph Layon, Jerome H. Modell, David S. Warner, Mark A. Warner; Drowning: Update 2009. Anesthesiology 2009; 110:1390–1401 do
4 Paz P, Makram J, Mallah H, Mantilla B, Ball S, Nugent K. Swimming-induced pulmonary edema. Proc (Bayl Univ Med Cent). 2020 Mar 9;33(3):409-412.
5 Datta A, Tipton M. Respiratory responses to cold water immersion: neural pathways, interactions, and clinical consequences awake and asleep. J Appl Physiol (1985). 2006;100(6):2057-2064.
6 Centers for Disease Control and Prevention. Definitions for Nonfatal Injury Reports | Nonfatal Injury Reports Help Menu | WISQARS | Injury Center. last reviewed: March 14, 2017.
7 Personal communication: Craig Nelson, M.D. Forensic Pathologist.
8 Ludlow CL. Laryngeal Reflexes: Physiology, Technique, and Clinical Use. J Clin Neurophysiol. 2015;32(4):284-293.
9 Orlowski JP, Szpilman D. Drowning. Rescue, resuscitation, and reanimation. Pediatr Clin North Am. 2001;48(3):627-646.
10 Bhalotra AR, Thakur P. Suction, No Suction or Passive Drainage for Pulmonary Oedema. Turk J Anaesthesiol Reanim. 2018;46(6):480-481. doi:10.5152/TJAR.2018.43179
11 Bierens JJ, Knape JT, Gelissen HP. Drowning. Curr Opin Crit Care. 2002;8(6):578-586.
12 Knudsen L, Ochs M. The micromechanics of lung alveoli: structure and function of surfactant and tissue components. Histochem Cell Biol. 2018 Dec;150(6):661-676
13 Seadler BD, Toro F, Sharma S. Physiology, Alveolar Tension. [Updated 2021 May 10]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2021 Jan-. https://www.ncbi.nlm.nih.gov/books/NBK539825/
14 Veldhuizen E. Haagsman H. Role of pulmonary surfactant components in surface film formation and dynamics, Biochimica et Biophysica Acta (BBA) – Biomembranes, 2002:Vol 1467; Issue 2; 255-270
15 Daniels C, Orgeig S. Pulmonary Surfactant: The Key to the Evolution of Air Breathing. 1 Aug 2003
16 Knudsen L, Ochs M. The micromechanics of lung alveoli: structure and function of surfactant and tissue components. Histochem Cell Biol. 2018;150(6):661-676. doi:10.1007/s00418-018-1747-9.
17 Han S, Mallampalli RK. The Role of Surfactant in Lung Disease and Host Defense against Pulmonary Infections. Ann Am Thorac Soc. 2015;12(5):765-774. doi:10.1513/AnnalsATS.201411-507FR.
18 Casals C, Cañadas O. Role of lipid ordered/disordered phase coexistence in pulmonary surfactant function. Biochimica et Biophysica Acta (BBA) – Biomembranes. 2012:Vol 1818; Issue 11: 2550-2562.
19 Meyer K. Exercise training in heart failure: recommendations based on current research Med Sci Sports Exerc 2001 33 4 525 531.
20 Iqbal MA, Gupta M. Cardiogenic Pulmonary Edema. [Updated 2020 Dec 16]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2021 page 1
21 Lunetta P, Modell JH, Sajantila A. What is the incidence and significance of “dry-lungs” in bodies found in water?. Am J Forensic Med Pathol. 2004;25(4):291-301
22 Oxford Languages: Parenchyma
23 Perlman CE, Lederer DJ, Bhattacharya J. Micromechanics of alveolar edema. Am J Respir Cell Mol Biol. 2011;44(1):34-39. doi:10.1165/rcmb.2009-0005OC
24 Modell JH, Davis JH. Electrolyte changes in human drowning victims. Anesthesiology. 1969;30(4):414.
25 Modell JH, Moya F. Effects of volume of aspirated fluid during chlorinated fresh water drowning. Anesthesiology. 1966;27(5):662.
26 Orlowski JP, Szpilman D. Drowning. Rescue, resuscitation, and reanimation. Pediatr Clin North Am. 2001;48(3):627-646.
27 Chandy D, Weinhouse G. Drowning (submersion injuries). UpToDate. 2020: June. https://www.uptodate.com/contents/drowning-submersion-injuries#H5
28 Battaglia JD, Lockhart CH. Drowning and near-drowning. Pediatr Ann. 1977;6(4):270.
29 Merriam-Webster: Morbidity
30 A Joseph Layon, Jerome H. Modell, David S. Warner, Mark A. Warner; Drowning: Update 2009. Anesthesiology 2009; 110:1390–1401
31 Cases reviewed by Walter Butch Hendrick and the author.
32 There are ~59.8 pints in 1 cuft. Therefore, if we round that to 60, each pint is equal to 1.07 lbs of seawater displacement.
33 Rounding from 63.93 cuft. https://www.aqua-calc.com/calculate/volume-to-weight
34 Volume to weight conversions
35 Lifeguard Systems, Inc www.teamlgs.com
36 Density vs. Specific Gravity Tek Tip. viewed June 5, 2021.
37 Ibid.
38 Water – Specific Gravity. The Engineering ToolBox. 2019
39 http://www.csgnetwork.com/h2odenscalc.html
40 Behnke A.R., Feen B.G., Welham W.C. The specific gravity of healthy men. Obesity Research May 1995 3(3): 295-300
41 Farvid M. S., Ng T.K., Chan D.C., Barrett P.R., Watts G.F., Association of adiponectin and resistin with adipose tissue compartments, insulin resistance and dyslipidaemia. Diabetes Obesity and Metabolism 7(4):406-13 · August 2005
42 Samuel R. Ward Richard L. Lieber. Density and hydration of fresh and fxed human skeletal. Muscle J of Bioemechanics November 2005 Volume 38, Issue 11, Pages 2317–2320
43 Cote C, Faulkner JA, 1984. Motor unit function in skeletal muscle autografts of rats. Exp Neurol 84:292-305
44 Yang J, Chiou R, Ruprecht A, Vicario J, MacPhail LA, Rams TE. A new device for measuring density of jaw bones. Dentomaxillofacial Radiology (2002) 31, 313 – 316
45 This is consistent with other findings. Edmonds, Carl; Thomas, Bob; McKenzie, Bart; Pennefather, John (2015). “Why divers die”(PDF). Diving Medicine for Scuba Divers. pp. Chapter 34.
46 https://www.dictionary.com/browse/incapacitation
47 M. J. Tipton; The Initial Responses to Cold-Water Immersion in Man. Clin Sci (Lond) 1 December 1989; 77 (6): 581–588
48 Giesbrecht GG. Cold stress, near drowning and accidental hypothermia: a review. Aviat Space Environ Med. 2000 Jul;71(7):733-52
49 Shattock MJ, Tipton MJ ‘Autonomic conflict’: a different way to die during cold water immersion? The J of physiol 590 (14), 3219-3230
50 The heart beat has an abnormal speed or rhythm.
51 Papadakis, M., Raju, H., Behr, E. R., De Noronha, S. V., Spath, N., Kouloubinis, A., Sheppard, M. N., & Sharma, S. (2013). Sudden cardiac death with autopsy findings of uncertain significance: potential for erroneous interpretation. Circulation. Arrhythmia and electrophysiology, 6(3), 588–596.
52 https://www.lexico.com/en/definition/panic
53Wikipedia: Panic
54 Clark JE. Moving in extreme environments: inert gas narcosis and underwater activities. Extreme Physiology & Medicine. 2015:4L1
55 Vincent MJ, Tipton MJ. The effects of cold immersion and hand protection on grip strength. Aviat Space Environ Med. 1988;59(8):738-741.
56 Vann R, Lang M. Recreational diving fatalities. Undersea & Hyperbaric Med J. 2011: 38(4):257-60
57 Denoble PJ, Caruso JL, Dear Gde L, Pieper CF, Vann RD. Common causes of open-circuit recreational diving fatalities. Undersea Hyperb Med. 2008;35(6):393-406.
58 Caruso J. The Pathologist’s approach to SCUBA diving deaths. American Society for Clinical Pathology Fall 2006 Teleconference series.
59 Including but not limited to witnesses, dive leaders, rescue personnel, law enforcement, dive experts, medical personnel, death investigators.
60 Authors Zaferes and Hendrick did not know of the Japanese man’s intentions and when he was presented to them as a patient, they performed CPR causing him to regain heartbeat, breathing, and consciousness during the 2-hour transport to the mainland where he died several hours later after the authors left him in a third world medical clinic.
61 The death was determined to be a homicide after a well-trained police diver, who recognized that the father’s story did not match the scene or circumstances, investigated the case and during the boy’s wake, the father confessed to him that he purposefully turned off his 16 year old son’s air to drown him. The father reported that his plan was to perform a suicide-homicide that for some reason only resulted in a homicide.
DIVE DEEPER
NYT: Drowning Is No. 1 Killer of Young Children. U.S. Efforts to Fix It Are Lagging by Emily Baumgaertner (JUL 2023) Thirty years of progress in decreasing drowning deaths in the United States appears to have plateaued, and disparities in deaths among some racial groups have worsened.
CDC: CDC Drowning Facts
Divers Alert Network (DAN): What Drowning Really Looks Like
Andrea Zaferes Workshop Series: The Pathophysiology of Drowning Workshop (5.5hrs.) Drowning is one of the most common forms of injury related deaths worldwide. This workshop presented by Andrea Zaferas covers the complex pathophysiology of the drowning process, terminology changes, myths, the diagnosis of drowning, epidemiology, and a current literature review.
Andrea Zaferes Forensic Workshop Series (5 hrs): Aquatic Crimes Against Women (ACAW) Homicides Staged as Drowning Accidents or Suicides online course.
Andrea Zaferes Forensic Workshop Series (3.5 hrs): Forensic Diving Fatality Investigation and Prevention

For more information on how to recognize, manage, and prevent problems such as drowning, as well as education on dozens of additional diving topics check out the more than 75 online workshops and webinars on The Diver Medic.
Divers Alert Network (DAN) Annual Diving Reports

Andrea Zaferas has been investigating aquatic deaths and teaching water rescue/recovery with Lifeguard Systems/TeamLGS, for over 30 years with Walt Butch Hendrick. She is a medicolegal death investigator with Dutchess County Medical Examiner’s office, and helped start a nonprofit organization—RIPTIDE—to conduct research, assist with submerged evidence/body recovery, and perform aquatic abuse and homicide investigations. She is an innovator in the field of aquatic and asphyxiation death, abuse, homicide, and sexual assault investigation, and has taught thousands of law enforcement, death investigators, jurisprudence members, medical personnel, and domestic violence workers how to recognize and investigate these cases.
Andrea has spoken at more than 120 forensic and 150 rescue/dive conferences worldwide, reviewed well over 1,500 aquatic cases, and is one of the leading public safety diving Instructors in the U.S. and Canada with several national awards. Seen on such programming as Dateline, 48 Hours, and National Geographic, Andrea is a member of the American Academy of Forensic Sciences, the International Association of County Coroners, and the Medical Examiners Association. She is a NAUI/ANDI Course Director and PADI Master Instructor, and has more than 100 publications. She serves as an aquatic death specialized-knowledge expert in aquatic homicide cases, is a pro bono consultant to the National Center for Missing and Exploited Children, and assists with adult and pediatric aquatic abuse and death investigations worldwide.