DCS
Deco Dilemmas: The Push for Personalized Decompression Modeling
By Reilly Fogarty. Photo credits as noted.
Limited technology, an absolute dearth of reproducible data, and the need for a repeatable and modifiable algorithm are all that stand between you and a personalized decompression model for your next dive. If it sounds like a lot—it is.
The stark reality is that the best and brightest minds in hyperbarics have spent their careers making—sometimes huge and often fascinating—advances in research that not only cannot be applied to the real world, but also cannot be correlated with any yet-identified physiologic or biologic metrics. We have strong evidence that decompression sickness (DCS) is caused by intracorporeal bubble formation resulting from supersaturated dissolved gas, but recent data suggests that the quantity of those bubbles alone is not enough to predict whether someone will experience DCS symptoms.1
Knowing what most likely causes DCS is a weak enough base to build a decompression algorithm on, but the issue is compounded on all fronts. Researchers have chased dozens of biometric markers in the hopes of correlating them with DCS symptoms, but none have managed to do so in a reliable way (at least not yet). Measuring these markers is difficult in a lab and, in most cases, impossible to monitor during a dive, and current decompression algorithms are not designed to take any of these metrics into consideration.
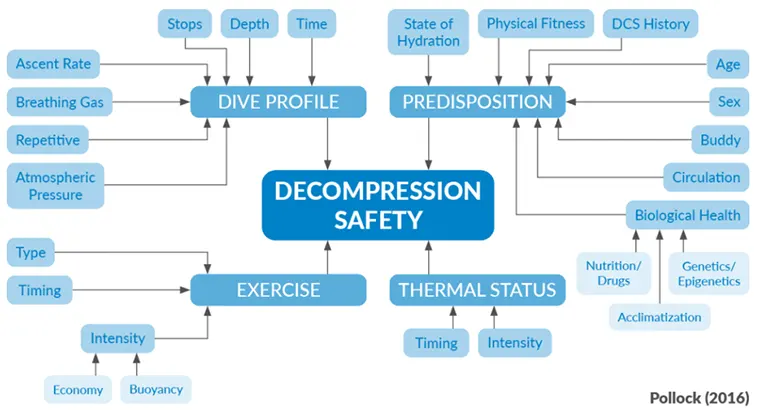
Having said all of that, some amount of personalized decompression modeling is possible now—but not in the way that most of us would expect. “The well-informed diver can personalize their practice by being mindful of what the dive computer algorithms know and do not know, and making adjustments based on real-time events and their experience, predispositions, and risk tolerance,” says Neal Pollock, Ph.D and expert in hyperbaric and diving research. It’s possible to modify your dive profile based on what we think will increase risk and, done well, this can do a great deal to minimize your chance of injury.
Making the leap from the probabilistic decompression algorithms we currently use to a deterministic model is going to require breakthroughs in decompression models, physiological monitoring tools, and our understanding of the physiology of decompression. It’s a tall order by any measure, but the potential for a single breakthrough to completely change our understanding of decompression modeling absolutely exists—and it’s what makes this research so exciting.
Dive deeper into what we know about personalized DCS modeling, what we need to know, and what research to keep an eye on:
Why Personalized Decompression Hasn’t Been Cracked – Yet.
The issues with decompression modeling start at a cellular level with our understanding of DCS. We think bubbles cause DCS symptoms, but there hasn’t yet been any solid data showing a correlation between bubble load or size and DCS. Complicating matters further, there’s a whole slew of research indicating that it might not be the bubbles causing injury but a body’s response to those bubbles2 (more on that later). Without an understanding of the mechanism of injury behind DCS, decompression algorithms become a probabilistic prediction of estimated risk rather than a predictive algorithm based on real-time data. Effectively, you’re still diving a model based on data derived from giving goats DCS more than a century ago. If the goats survived the dive, then you probably would too.
Applied with enough conservatism, this can offer a relative level of safety to divers but without any real way to quantify that risk. Relative is doing the heavy lifting in this description, and the crux of the issue is that we have no way of knowing how safe you’ll be following a dive profile even with the added conservatism—without a way to understand and quantify DCS risk, we’re effectively shooting in the dark. Our current algorithms are rudimentary at best but “staggeringly incapable of assessing a host of complex factors and timings that can influence gas uptake, elimination, and effective risk,” says Pollock, adding that decompression algorithms are useful for a “first order approximation of risk—getting into the ballpark.” Beyond this point, Pollock advocates for divers to use algorithms as a base upon which to make conservative modifications based on experience and research, even though there will inevitably be a lot of supposition and guesswork.

The next hurdles for researchers are the metrics we use to measure DCS risk. Personalizing decompression requires measuring something about a diver—whether that be temperature or hydration status, epigenetic markers, or one of dozens of other possible physiological or biological markers. It’s generally accepted that exercise and thermal status before, during, and after the dive3,4 are likely the strongest measurable physiological factors affecting DCS risk; but the effects on DCS risk are relative, and no decompression algorithms exist that can consider them.
Beyond these, there are an endless number of proposed physiological, genetic, or biological metrics without any experimental data to support them, as well as a number of promising factors that haven’t been adequately explored yet. These range from concrete microparticle measurements and solid but abstract joint motion and force metrics to the truly bizarre. Fascinating to research but difficult to quantify, these represent the most interesting area of this conundrum for most divers.
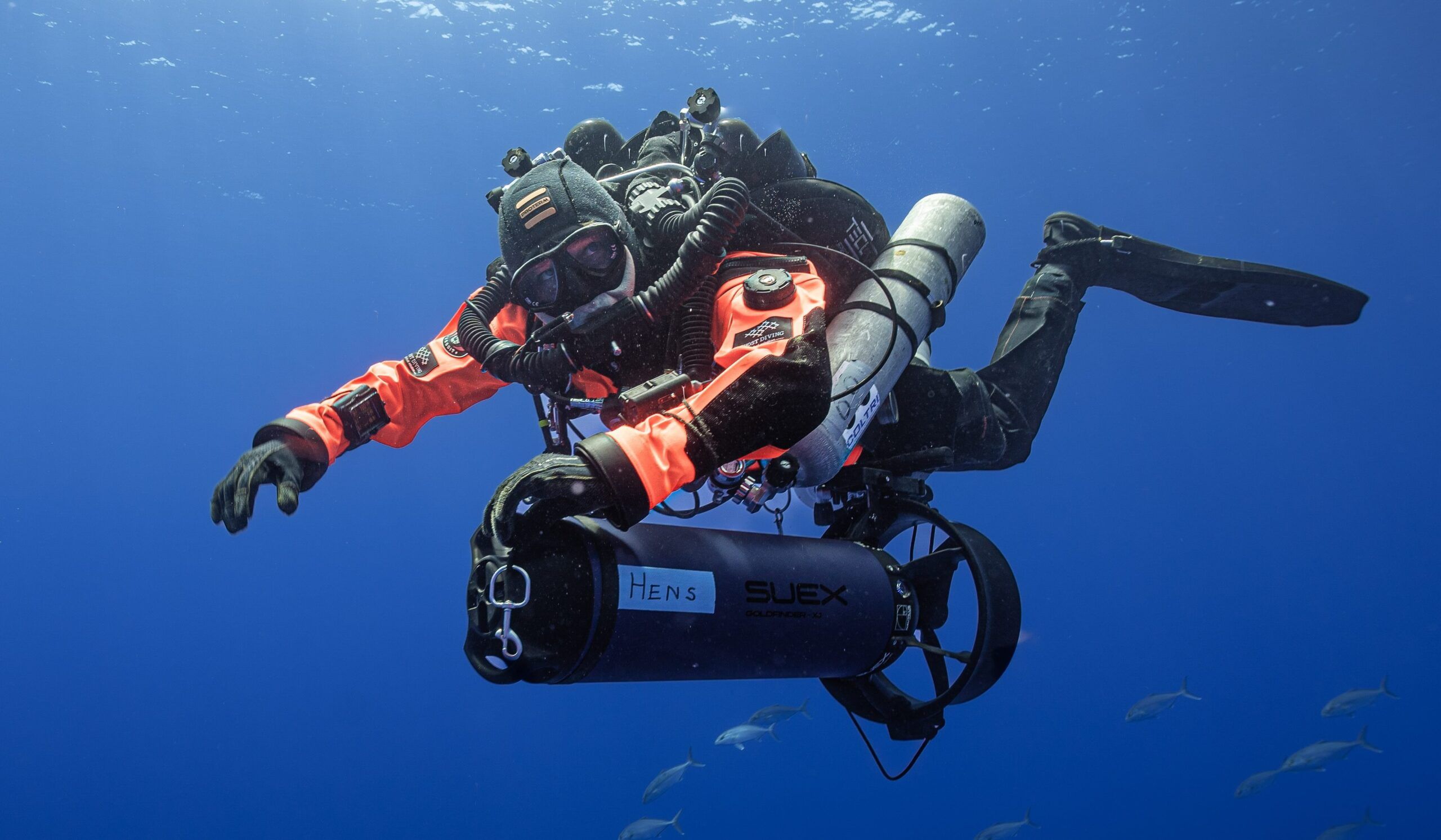
The final hurdle on the road to personalized decompression is the lack of existing technology to measure these markers. Many (but not all) of these biomarkers can be measured with currently available technology, but virtually none can be tracked during a dive, and few can be easily assessed outside of a well-funded lab. Not only will several biomarkers have to be identified and correlated with DCS risk, but the technology will have to be developed to monitor them throughout the dive in a reproducible way. And then that data must be presented to a yet-undeveloped algorithm capable of modifying a dive profile in real-time based on the direction of trending data.
Lacking the algorithm, biomarkers, and technology to measure any of the above, there may still be hope. “We don’t know what we don’t know,” contends Frauke Tillmans, Ph.D, VP of Research at Divers Alert Network. “That is to say that we know a lot, and there is a lot of exciting research ongoing, but we don’t yet know the questions to ask to move in the right direction.” The hope is that, despite not knowing which research to focus on specifically, each study will build a broad enough base to further the rest of the field.
Divers Alert Network (DAN), researchers at Duke University, the Navy Experimental Dive Unit (NEDU), and the Undersea and Hyperbaric Medical Society (UHMS) all have ongoing projects with promising preliminary results in this area of study, but it’s important to recognize that research is a slow process, and even studies that confirm a negative result or disprove an exciting hypothesis still advance the field.
Personalizing your decompression algorithm and reducing your risk of DCS in a meaningful way may not be possible by the time you hit the water next, but there’s a very real chance of one or even several of these ongoing studies causing a complete evolution in the way we manage diver risk in the relatively near future.
Factors with a Future
Algorithms and new monitoring tools are fun to build, but the truly thrilling part of all of this is the research into new DCS risk factors and markers that could correlate with DCS risk—or even lead to a real understanding of the mechanism of DCS. There are too many of these to count, and it’s impossible to know which (if any) will ultimately provide real insight into why we bubble the way we do, but the potential for breakthrough feels tantalizingly close to some in the field. This is by no means a complete summary of the field, but here’s what we know right now (and the research you should be watching in the coming years).
Diver Pre-Conditioning
First off the block is diver pre-conditioning. This is a bit of a backwards approach—there aren’t many metrics or modifiers for future algorithms here. Instead, pre-conditioning focuses on modifying diver behavior before, during, or after a dive. Exercise, medications, and foods that might minimize inflammatory response fall into this category. The more abstract projects here focus on things like bouncing on a trampoline before a dive, eating dark chocolate, and heat exposure in a sauna3,4. These make for an excellent pre-dive ritual on a cold morning, but these are either entirely theoretical approaches or they currently lack a useful dataset.
Exercise is one pre-conditioning factor with a more solid data-set to work with. There is some evidence that aerobic exercise within 24 hours pre-dive may reduce DCS risk5, and human studies have shown a demonstrably reduced venous gas embolism (VGE) formation after dives performed following a high-intensity exercise protocol. These exercise protocols also showed a somewhat reduced post-dive microparticle production and neutrophil activation (a measure of inflammatory response)6,7,8. Unfortunately, pre-dive exercise has not been subject to a large controlled study yet, and there is some research to indicate that exercise performed during and after a dive can increase DCS risk.
There’s an interesting crossover in this area with some of the project dedicated to exploring adjunctive treatments for DCS [Link to Reilly article!]. These largely suffer from the same lack of data, but it stands to reason that some medications or supplements used to minimize inflammatory processes or improve off-gassing could offer benefits in DCS prevention as well as treatment of DCS symptoms. Pre-breathing oxygen9,10 and exogenous nitric oxide administration11 before a dive have both shown promise in reducing VGE load in divers but, similarly, suffer from a lack of adequate data and the lack of defined correlation between VGE load and DCS symptoms.
Hydration and Temperature
On the whole, dive instructors have done a decent job of teaching new students the importance of hydration and temperature management before dives. In terms of monitoring both of these during a dive—we’re not quite there yet.
Hydration is anecdotally accepted as an important factor in DCS risk, but there are no human studies showing that pre-dive hydration reduces DCS. There is a balance to be struck between too much and too little water, however: Dehydration likely increases DCS risk while over-hydration may increase risk of immersion pulmonary edema (IPE). The biggest current hurdle with hydration status is quantifying it and then applying that metric in some meaningful way to a decompression algorithm12.
Diver temperature is somewhat easier to measure in-water but suffers from similar lack of meaningful application. Accessibility of heated undergarments has made this a hot topic in the technical diving community, but what data we do have is still conflicted. In theory, improving perfusion during decompression will improve off-gassing, but this is complicated by the increased tissue saturation at depth when using heated undergarments and the potential for heat to fail only after being used at depth—potentially increasing tissue gas load but reducing ability to release that gas during decompression.

Microparticles and Inflammatory Response
There’s a growing body of research suggesting that some of the harm caused by DCS is done not by mechanical damage from VGE formation during decompression but, instead, by microparticles caused by bubble formation and the inflammatory responses to both the bubbles and the microparticles.13,14. The proposed mechanisms for microparticle and inflammatory response to decompression and their contributions to DCS risk are somewhat convoluted and could be the subject of their own article, but an excellent summary can be found in Decompression Illness: A Comprehensive Overview,1. a 2024 summary by expert in the field Dr. Simon Mitchell.
Microparticles and the inflammatory cytokines that these theories focus on can be measured—but only in a lab and not in real-time. More work needs to be done in this area to determine the relationship between oxidative stress, decompression, and circulating microparticles before meaningful progress can be made, but the interplay between the three and the data that does exist makes this a topic to pay particular attention to in the coming years.
Bubble Studies
Bubbles and decompression sickness may be impossible to separate after so many decades of suggestive (but not conclusive) findings, but a recent study from the NEDU and the University of Auckland may have put the final nail in the coffin connecting VGE loads and DCS. If you, like most of us, follow academic hyperbaric research for the drama, Within-diver variability in venous gas emboli (VGE) following repeated dives1 has all the thrills and excitement you could hope for.
While the diving community has been placing high hopes on studies that count VGE formation post-dive for decades, there has always been a disconnect between VGE loads and DCS symptoms. Last year, principal researchers Doolette and Murphy took 151 divers and put them through repeatable dive profiles under controlled conditions, measured their VGE grades, and then repeated the exercise 693 times. The result was a uniquely large data set for this area of research, and one that strongly suggests that the variability of VGE grades is great enough that not only can we not use them to evaluate decompression practices between divers but that individual divers on identical dives will bubble at such varying rates that VGE grade may not have any meaningful correlation with DCS at all.
This throws a bit of a monkey wrench in the world of personal bubble-count devices and studies focusing on bubble load, but it’s not the end of bubble counting. DAN researchers have recently finished a four-year data collection project aimed partially at quantifying VGE load variability and building on the Doolette and Murphy paper. Data crunching has just begun, but the project also looked at metrics like heart rate, cardiac output, blood pressure, saliva samples for inflammatory markers, and blood samples for microparticles. In the short term, data analysis will focus on correlation between DCS risk factors and bubble counts—not bubble counts and DCS—but the project has also created a cohort of divers and researchers capable of performing repeatable dives under laboratory conditions. The combination means that researchers can pivot future projects to focus on what results may come out of the current data set and much more quickly and reliably test future theories.

Looking To the Future
Despite much of this research hinging on still unproven mechanisms of DCS—yet-undeveloped technology and algorithms that aren’t yet a twinkle in their developer’s brain—there are a lot of reasons to be optimistic. While we must temper that optimism with the knowledge that it may be years before the technology even exists to measure some of these theoretical markers in a meaningful way, it’s hard not to get excited about the sheer number of possibilities in this area.
Personalized decompression may not yet be a reality, but the hurdles to get there are identifiable, and some brilliant researchers and divers are devoting their lives to making it possible. Interested in advancing the cause? You can learn about ongoing DAN research projects and volunteer to help at: Current Research.
Return to The State of Personalized Decompression.
Works Cited
- Doolette, D; Murphy, G (2023) Within-diver variability in venous gas emboli (VGE) following repeated dives.
- Mitchell, Simon J (2024) Decompression Illness: A comprehensive review. PMID: 38537300
- Lambrechts K, Germonpré P, Vandenheede J, Delorme M, Lafère P, Balestra C. Mini Trampoline, a new and promising way of SCUBA diving preconditioning to reduce vascular gas emboli? Int J Environ Res Public Health. 2022;19(9):5410. doi: 10.3390/ijerph19095410. PMID: 35564805. PMCID: PMC9105492.
- Germonpré P, Balestra C. Preconditioning to reduce decompression stress in scuba divers. Aerosp Med Hum Perform. 2017;88:114−20. doi: 10.3357/AMHP.4642.2017. PMID: 28095955.
- Wisløff U, Brubakk AO. Aerobic endurance training reduces bubble formation and increases survival in rats exposed to hyperbaric pressure. J Physiol. 2001;537(Pt 2):607–11. doi: 10.1111/j.1469-7793.2001.00607.x. PMID: 11731590. PMCID: PMC2278955.
- 173 Dujic Z, Duplancic D, Marinovic-Terzic I, Bakovic D, Ivancev V, Valic Z, et al. Aerobic exercise before diving reduces venous gas bubble formation in humans. J Physiol. 2004;555(Pt 3):637–42. doi: 10.1113/jphysiol.2003.059360. PMID: 14755001. PMCID: PMC1664874.
- 174 Blatteau JE, Gempp E, Galland FM, Pontier JM, Sainty JM, Robinet C. Aerobic exercise 2 hours before a dive to 30 msw decreases bubble formation after decompression. Aviat Space Environ Med. 2005;76:666−9. PMID: 16018350.
- 175 Castagna O, Brisswalter J, Vallee N, Blatteau JE. Endurance exercise immediately before sea diving reduces bubble formation in scuba divers. Eur J Appl Physiol. 2011;111:1047−54. doi: 10.1007/s00421-010-1723-0. PMID: 21107599.
- Castagna O, Gempp E, Blatteau J-E. Pre-dive normobaric oxygen reduces bubble formation in scuba divers. Eur J Appl Physiol. 2009;106:167–72. doi: 10.1007/s00421-009-1003-z. PMID: 19219451.
- 181 Bosco G, Yang ZJ, Di Tano G, Camporesi EM, Faralli F, Savini F, et al. Effect of in-water oxygen prebreathing at different depths on decompression-induced bubble formation and platelet activation. J Appl Physiol (1985). 2010;108:1077−83. doi: 10.1152/japplphysiol.01058.2009. PMID: 20185629.
- 182 Dujić Z, Palada I, Valic Z, Duplancić D, Obad A, Wisløff U, et al. Exogenous nitric oxide and bubble formation in divers. Med Sci Sports Exerc. 2006;38:1432−5. doi: 10.1249/01. mss.0000228936.78916.23. PMID: 16888456
- Shupak A, Weiler-Ravell D, Adir Y, Daskalovic YI, Ramon Y, Kerem D. Pulmonary oedema induced by strenuous swimming: a field study. Respir Physiol. 2000;121:25–31. doi: 10.1016/s0034-5687(00)00109-2. PMID: 10854620.
- Yu X, Xu J, Liu W, Xu W. Bubbles induce endothelial microparticle formation via a calcium-dependent pathway involving flippase inactivation and rho kinase activation. Cell Physiol Biochem. 2018;46:965–74. doi: 10.1159/000488825. PMID: 29669319.
- Helps SC, Gorman DF. Air embolism of the brain in rabbits pre-treated with mechlorethamine. Stroke. 1991;22:351–4. doi: 10.1161/01.str.22.3.351. PMID: 2003304.
DIVE DEEPER
Diving Hyperb Med: Decompression Illness: A Comprehensive Overview by Simon J Mitchell Volume 54 No 1 supplement, March 2024
Diving Hyperb Med: Venous gas emboli detected by two-dimensional echocardiography are an imperfect surrogate endpoint for decompression sickness by David Doolette
Diving Hyperb Med: Within-diver variability in venous gas emboli (VGE) following repeated dives. By David Doolette and Greg Murphy
InDEPTH: What is Undeserved in “Undeserved Decompression Sickness?” by Neal Pollock
InDEPTH: Dial In Your DCS Risk with the Thalmann Algorithm by Tim Blömeke
InDEPTH: Heart Rate Variability: What it is and Why it Matters by Sergio Rhein Schirato, PhD
InDEPTH: The Making of the Biometric Diver: DAN Europe’s Alessandro Marroni is Realizing a 50-year old Dream by Michael Menduno
InDEPTH: Oh Deco, Oh Doppler, O’Dive: Assessing the World’s First Personal Deco Safety Tool by Michael Menduno
InDEPTH: Decompression, Deep Stops, and the Pursuit of Precision in a Complex World by Jarrod Jablonski

Reilly Fogarty is an expert in diving safety, hyperbaric research, and risk management. Recent work has included research at the Duke Center for Hyperbaric Medicine and Environmental Physiology, risk management program creation at Divers Alert Network, and emergency simulation training for Harvard Medical School. A USCG licensed captain, he can most often be found running technical charters and teaching rebreather diving in Gloucester, Massachusetts.