Education
Understanding Oxygen Toxicity: Part 1 – Looking Back
In this first of a two-part series, Diver Alert Network’s Reilly Fogarty examines the research that has led to our current working understanding of oxygen toxicity. He presents the history of oxygen toxicity research, our current toxicity models, the external risk factors we now understand, and what the future of this research will look like. Mind your PO2s!

By Reilly Fogarty
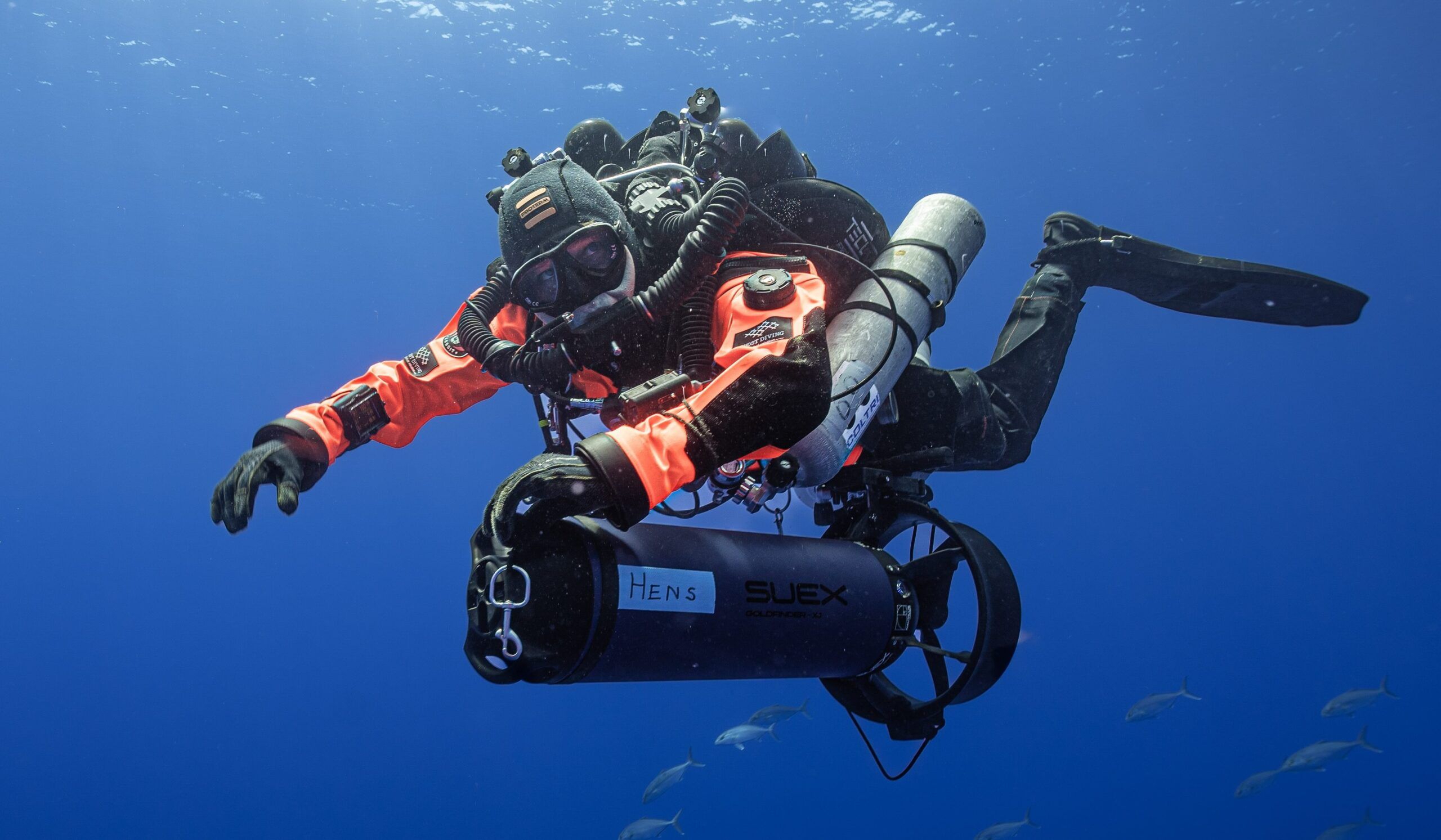
Header photo courtesy of DAN
Oxygen toxicity is a controversial subject among researchers and an intimidating one for many divers. From the heyday of the “voodoo gas” debates in the early 1990s to the cursory introduction to oxygen-induced seizure evolution that most divers receive in dive courses, the manifestations of prolonged or severe hyperoxia can often seem like a mysterious source of danger.
Although oxygen can do great harm, its appropriate use can extend divers’ limits and improve the treatment of injured divers. The limits of human exposure are tumultuous, often far greater than theorized, but occasionally–and unpredictably–far less.
Discussions of oxygen toxicity refer primarily to two specific manifestations of symptoms: those affecting the central nervous system (CNS) and those affecting the pulmonary system. Both are correlated (by different models) to exposure to elevated partial pressure of oxygen (PO2). CNS toxicity causes symptoms such as vertigo, twitching, sensations of abnormality, visual or acoustic hallucinations, and convulsions. Pulmonary toxicity primarily results in irritation of the airway and lungs and decline in lung function that can lead to alveolar damage and, ultimately, loss of function.
The multitude of reactions that takes place in the human body, combined with external risk factors, physiological differences, and differences in application, can make the type and severity of reactions to hyperoxia hugely variable. Combine this with a body of research that has not advanced much since 1986, a small cadre of researchers who study these effects as they pertain to diving, and an even smaller group who perform research available to the public, and efforts to get a better understanding of oxygen toxicity can become an exercise in frustration.
Piecing together a working understanding involves recognizing where the research began, understanding oxygen toxicity (and model risk for it) now, and considering the factors that make modeling difficult and increase the risk. This article is the first in a two-part series. It will cover the history of oxygen toxicity research, our current models, the external risk factors we understand now, and what the future of this research will look like.
Early Research
After oxygen was discovered by Carl Scheele in 1772, it took just under a century for researchers to discover that, while the gas is necessary for critical physiological functions, it can be lethal in some environments. The first recorded research on this dates back to 1865, when French physiologist Paul Bert noted that “oxygen at a certain elevation of pressure, becomes formidable, often deadly, for all animal life” (Shykoff, 2019). Just 34 years later, James Lorrain Smith was working with John Scott Haldane in Belfast, researching respiratory physiology, when he noted that oxygen at “up to 41 percent of an atmosphere” was well-tolerated by mice, but at twice that pressure mouse mortality reached 50 percent, and at three times that pressure it was uniformly fatal (Hedley-White, 2008).
Interest in oxygen exposure up to this point was largely medical in nature. Researchers were physiologists and physicians working to understand the mechanics of oxygen metabolism and the treatment of various conditions. World War II and the advent of modern oxygen rebreathers brought the gas into the sights of the military, with both Allied and Axis forces researching the effects of oxygen on divers. Chris Lambertsen developed the Lambertsen Amphibious Respiratory Unit (LARU), a self-contained rebreather system using oxygen and a CO2 absorbent to extend the abilities of U.S. Army soldiers, and personally survived four recorded oxygen-induced seizures.
Kenneth Donald, a British physician, began work in 1942 to investigate cases of loss of consciousness reported by British Royal Navy divers using similar devices. In approximately 2,000 trials, Donald experimented with PO2 exposures of 1.8 to 3.7 bar, noting that the dangers of oxygen toxicity were “far greater than was previously realized … making diving on pure oxygen below 25 feet of sea water a hazardous gamble” (Shykoff, 2019). While this marked the beginning of the body of research that resembles what we reference now, Donald also noted that “the variation of symptoms even in the same individual, and at times their complete absence before convulsions, constitute[d] a grave menace to the independent oxygen-diver” (Shykoff, 2019). He made note not just of the toxic nature of oxygen but also the enormous variability in symptom onset, even in the same diver from day to day.
The U.S. Navy Experimental Diving Unit (NEDU), among other groups in the United States and elsewhere, worked to expand that understanding with multiple decades-long studies. These studies looked at CNS toxicity in: immersed subjects with a PO2 of less than 1.8 from 1947 to 1986; pulmonary toxicity (immersed, with a PO2 of 1.3 to 1.6 bar, and dry from 1.6 to 2 bar) from 2000 to 2015; and whole-body effects of long exposures at a PO2 of 1.3 from 2008 until this year.
The Duke Center for Hyperbaric Medicine and Environmental Physiology, the University of Pennsylvania, and numerous other groups have performed concurrent studies on similar topics, with the trend being a focus on understanding how and why divers experience oxygen toxicity symptoms and what the safe limits of oxygen exposure are. Those limits have markedly decreased from their initial proposals, with Butler and Thalmann proposing a limit of 240 minutes on oxygen at or above 25 ft/8 m and 80 minutes at 30 ft/9 m, to the modern recommendation of no greater than 45 minutes at a PO2 of 1.6 (the PO2 of pure oxygen at 20 ft/6 m).
Between 1935 and 1986, dozens of studies were performed looking at oxygen toxicity in various facets, with exposures both mild and moderate, in chambers both wet and dry. After 1986, these original hyperbaric studies almost universally ended, and the bulk of research we have to work with comes from before 1986. For the most part, research after this time has been extrapolated from previously recorded data, and, until very recently, lack of funding and industry direction coupled with risk and logistical concerns have hampered original studies from expanding our understanding of oxygen toxicity.
Primary Toxicity Models
What we’re left with are three primary models to predict the effects of both CNS and pulmonary oxygen toxicity. Two models originate in papers published by researchers working out of the Naval Medical Research Institute in Bethesda, Maryland, in 1995 (Harabin et al., 1993, 1995), and one in 2003 from the Israel Naval Medical Institute in Haifa (Arieli, 2003). The Harabin papers propose two models, one of which fits the risk of oxygen toxicity to an exponential model that links the risk of symptom development to partial pressure, time of exposure, and depth (Harabin et al., 1993). The other uses an autocatalytic model to perform a similar risk estimate on a model that includes periodic exposure decreases (time spent at a lower PO2). The Arieli model focuses on many of the same variables but attempts to add the effects of metabolic rate and CO2 to the risk prediction. Each of these three models appears to fit the raw data well but fails when compared to data sets in which external factors were controlled.
Comparison of predicted and recorded oxygen toxicity incidents by proposed model (Shykoff, 2019).
The culmination of all this work and modeling is that we now have a reasonable understanding of a few things. First, CNS toxicity is rare at low PO2, so modeling is difficult but risk is similarly low. Second, most current models overestimate risk above a PO2 of 1.7 (Shykoff, 2019). This does not mean that high partial pressures of oxygen are without risk (experience has shown that they do pose significant risk), but the models cannot accurately predict that risk. Finally, although we cannot directly estimate risk based on the data we currently have, most applications should limit PO2 to less than 1.7 bar (Shykoff, 2019).
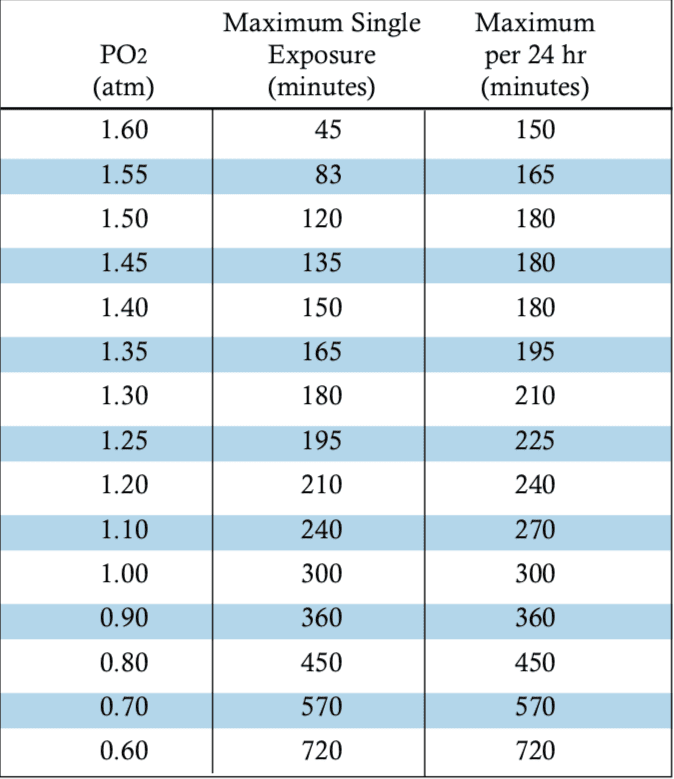
For the majority of divers, the National Oceanic and Atmospheric Administration’s (NOAA) oxygen exposure recommendations remain a conservative and well-respected choice for consideration of limitations. The research we do have appears to show that these exposure limits are safe in the majority of applications, and despite the controversy over risk modeling and variability in symptom evolution, planning dives using relatively conservative exposures such as those found in the NOAA table provides some measure of safety.
The crux of the issue in understanding oxygen toxicity appears to be the lack of a definitive mechanism for the contributing factors that play into risk predictions. There is an enormous variability of response to hyperoxia among individuals–even between the same individuals on different days. There are multiple potential pathways for injury and distinct differences between moderate and high PO2 exposures, and the extent of injuries and changes in the body are both difficult to measure and not yet fully understood.
Interested in the factors that play into oxygen toxicity risk and what the future of this research holds? We’ll cover that and more in the second part of this article in next month’s edition of InDepth.
Dive Deeper:
- Shykoff, B. (2019). Oxygen Toxicity: Existing models, existing data. Presented during EUBS 2019 proceedings.
- Hedley-Whyte, John. (2008). Pulmonary Oxygen Toxicity: Investigation and Mentoring. The Ulster Medical Journal 77(1): 39-42.
- Harabin, A. L., Survanshi, S. S., & Homer, L. D. (1995, May). A model for predicting central nervous system oxygen toxicity from hyperbaric oxygen exposures in humans.
- Harabin, A. L., Survanshi, S. S. (1993). A statistical analysis of recent naval experimental diving unit (NEDU) single-depth human exposures to 100% oxygen at pressure. Retrieved from https://apps.dtic.mil/dtic/tr/fulltext/u2/a273488.pdf
- Arieli, R. (2003, June). Model of CNS O2 toxicity in complex dives with varied metabolic rates and inspired CO2 levels.
- NOAA Diving Manual. (2001).
Part Two: Understanding Oxygen Toxicity Part II: Hypotheses and Hyperoxia
Two Fun (Math) Things:
CALCULATOR FOR ESTIMATING THE RISK OF PULMONARY OXYGEN TOXICITY by Dr. Barbara Shykoff
The Theoretical Diver: Calculating Oxygen CNS toxicity


Reilly Fogarty is a team leader for risk mitigation initiatives at Divers Alert Network (DAN). When not working on safety programs for DAN, he can be found running technical charters and teaching rebreather diving in Gloucester, MA. Reilly is a USCG licensed captain whose professional background includes surgical and wilderness emergency medicine as well as dive shop management.