Equipment
Oh Deco, Oh Doppler, O’Dive: Assessing the World’s First Personal Deco Safety Tool
Retired French Naval officer Axel Barbaud estimates that his company’s new product dubbed “O’Dive”—an innovative personalized safety tool—has the potential to reduce the diving community’s risk of DCS by a factor of five! Never mind that the exact incidence of DCS is unknown. What is known, is that O’Dive’s smart ultrasound sensor potentially represents a breakthrough in Doppler technology that has been sought after for more than 30 years.

By Michael Menduno
“If I asked you where the hell we were,” said Arthur weakly, “Would I regret it?” Ford stood up. “We’re safe,” he said. “Oh good,” said Arthur. “We’re in a small galley cabin in one of the space ships of the Vogon Constructor Fleet,” said Ford. “Ah, said Arthur, “this is obviously some strange usage of the word ‘safe’ that I wasn’t previously aware of.” Douglas Adams, The Hitchhiker’s Guide to the Universe
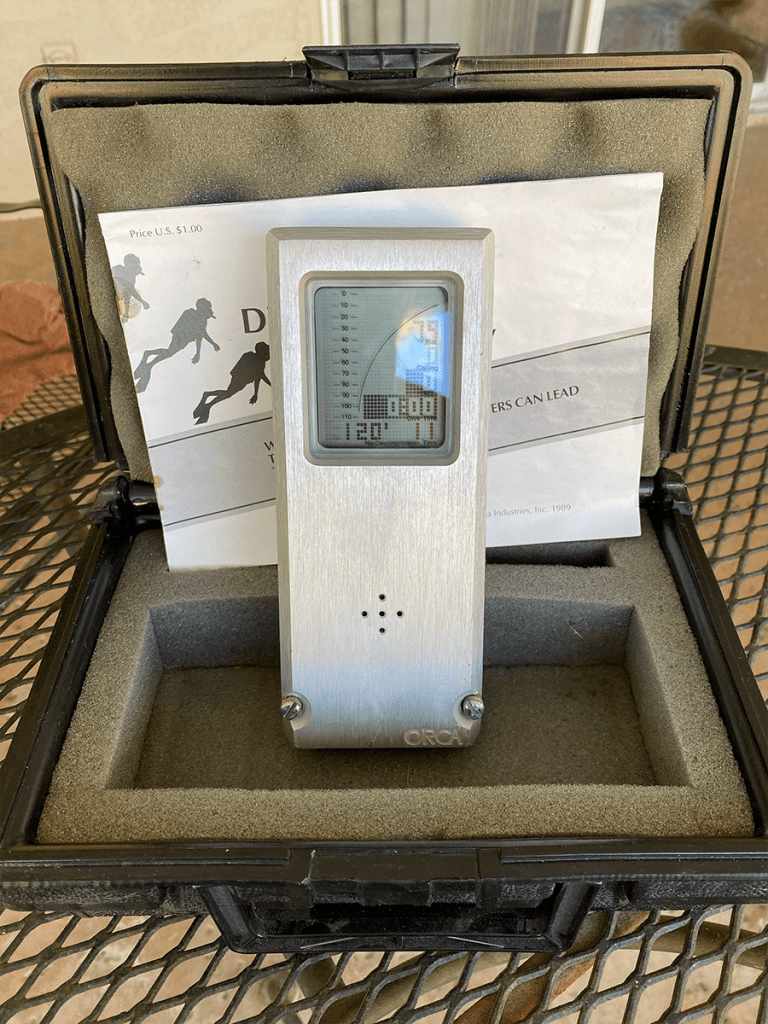
Every so often, someone invents a paradigm-shifting product that changes the way we view the world, and consequently, the way we behave. In 1983, ORCA Industries launched the “EDGE” Electronic Dive Guide, the first computational1 personal dive computer. In doing so, ORCA created a new approach to managing multilevel dive decompression, which arguably revolutionized sport diving and improved diving safety.
Similarly, in 1970, Dr. Merrill P. Spencer introduced the Spencer Precordial Bubble Detector, the first Doppler ultrasonic bubble detection device for divers, which enabled researchers to measure venous gas emboli (VGE) circulating in divers’ blood vessels. Though never a consumer item due to their expense and the expertise required to use them, Doppler monitoring technology has deepened our understanding of decompression sickness (DCS). It has also been a powerful tool for calibrating decompression tables and algorithms, including the algorithm developed by Karl Huggins for the EDGE.
Now a French company, Azoth Systems is hoping to achieve a similar distinction with a unique, innovative product called O’Dive, “The First Connected Sensor for Personalized Dives,” that couples statistical decompression analysis with Doppler ultrasound bubble detection, in order to improve diving safety. The company had a soft launch of the product last year and exhibited at the Paris International Dive Show in January, and also at the BOOT show in Düsseldorf, Germany. As of summer 2020, Azoth said it had about 1,000 O’Dive users in more than 25 countries.

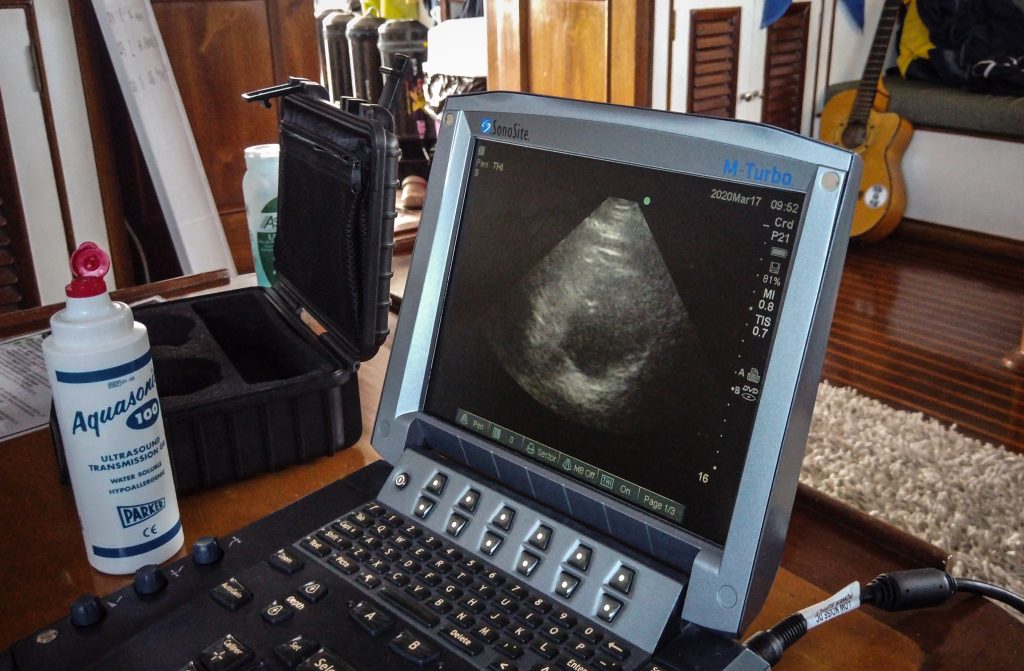
The device and its associated phone or tablet app purportedly enable a diver to measure the “quality of their decompression” on a scale from zero to 100%, based on an analysis of their dive profile along with the results of the post-dive bubble measurements taken with O’Dive’s subclavian Doppler monitor. Designed for divers to take their own measurements, the smart, hockey puck-sized Doppler sensor that uploads bubble measurement data to the cloud where it is automatically graded, hopes to provide a breakthrough in Doppler monitoring, one that has been sought for more than 30 years. Until now, taking a post-dive Doppler measurement required a trained technician to take an accurate reading and interpret the results.
But O’Dive goes further. With their decompression quality index on screen, the diver can query O’Dive’s predictive “what-if” model to determine if—and by how much—they could improve their decompression, by adjusting various factors of the dive, including the fractions of oxygen and helium in their gas mixes, the set point (in the case of a CCR dive), low and high gradient factors (GFs), addition of an extra decompression stop, and/or an adjustment of the length of the last stop. The diver could then incorporate preferred changes on subsequent dives, enabling them to improve their diving safety. Or so the theory goes.
“The primary goal of the tool is to help divers adjust their practice to progressively lower their bubble scores,” explained 50-year-old Azoth founder and CEO Axel Barbaud, who says that his key insight was to combine the risk assessment of a dive profile with post-dive bubble measurements to create a new predictive approach. He and his team estimate that O’Dive has the potential to reduce the community’s overall risk of DCS by a factor of five.
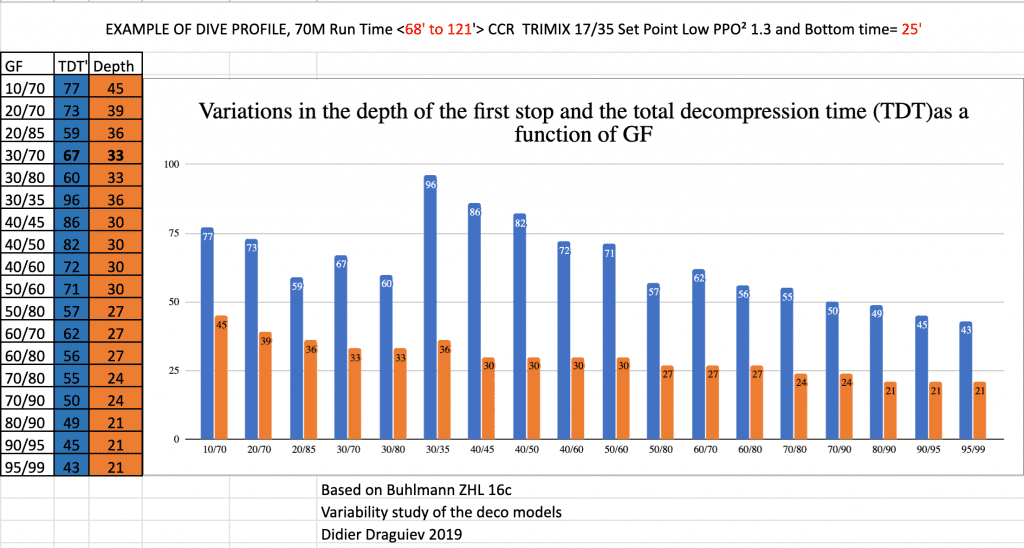
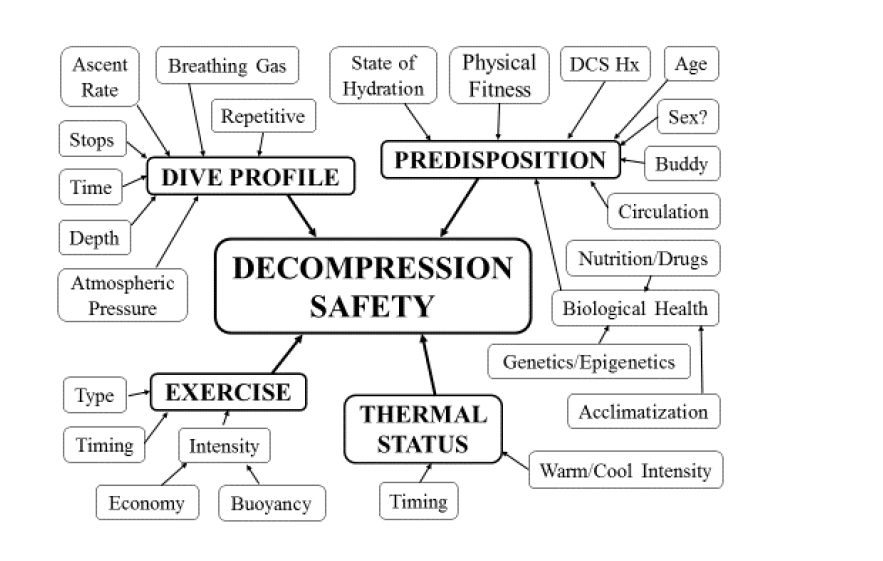
That may be tricky given that the exact incidence of DCS is unknown. However, it is a relatively rare occurrence with incident rates ranging from about 0.01%-0.1% per dive within the recreational, technical, scientific, military, and commercial diving communities.2 The problem is that many incidents occur in divers who reportedly followed their table or dive computer correctly—optimistically called “unprovoked hits.” These incidents might be partially explained by the variability of dive computer algorithms with user-adjustable settings even for the same dive (see Figure 1), but it also demonstrates that procedures do not account for individual susceptibility. That is the problem that Azoth Systems hopes to address with O’Dive.
Whether the product will be able to live up to its claims and actually improve divers’ safety is yet to be determined, and more evidence and experience will be required to demonstrate that O’Dive’s measurement and predictive systems are effective. “While I am aware of the O’Dive system, and think it important to develop these devices, I believe that optimism regarding its performance is premature. The validity of the tools must be assessed,” cautioned Neal Pollock, an Associate Professor in Kinesiology at Université Laval in Québec, Canada.
The Word on Dive Street

Almost everyone I spoke to who was familiar with O’Dive thought that the concept was brilliant. Diving educators, most of whom had obtained and had a chance to use O’Dive just before the “lockdown,” were clearly enthusiastic. “Azoth has created a phenomenal tool. I think it’s the biggest game changer since the personal dive computer,” exclaimed Paul Toomer, president of RAID who said that his agency will soon offer a training course for users. ”I was pretty much blown away by it,” admitted his colleague, instructor trainer Edd Stockdale, who is currently writing the course. “As a scientist, I just geek out on this stuff.”
RAID’s course will not be the first. The International Association of Nitrox and Technical Divers (IANTD) launched its own O’Dive training program in June, led by President of IANTD Indo-Pacific and IANTD board member Christian Heylen, who has conducted and supervised more than a hundred dives using O’Dive prototypes and the current unit over the last year. “O’Dive is the missing link in diving research, particularly in the absence of human experimentation. I think it’s the next step forward in revolutionizing diving safety and decompression,” he said, referring to the large amount of user data that Azoth will accumulate, which may aid future decompression research.

While excited about the product, veteran explorer and educator Phil Short expressed some concern that divers might misuse the device out of ignorance or willfulness. “The O’Dive concept is extraordinary. I just worry that the average diver may not know enough to interpret and understand numbers and do something safe with the information. Some might even use its predictive technology to see how far they could push the limits. On the other hand, if all O’Dive did was provide bubble readings, I don’t know if divers would buy it,” Short said referring to O’Dive’s what-if capability.
Interestingly, while most diving researchers and a dive computer executive I spoke with lauded O’Dive’s Doppler monitor, they were noticeably uncomfortable with the app’s underlying predictive model, which seemingly offers a high degree of precision in a field historically awash in uncertainty. One diving physiologist turned tech diver who was clearly skeptical about Azoth’s claims, called O’Dive a brilliant “marketing” concept: “It’s exactly the kind of techno-babble that techies buy into,” he said.
Divers Alert Network’s (DAN) US Research Director Frauke Tillmans is conducting one of the first comparative studies of three different Doppler devices including two precordial 2D-ultrasound devices and O’Dive’s subclavian sensor. The study was temporarily put on hold due to the pandemic. She refers to O’Dive as a black box. “I think Azoth’s subclavian approach is valid. It appears to be a reliable measurement technology. But we don’t know if safety is improved,” Tillmans told me.

DAN Europe’s Vice President of Research and Education, Professor Costantino Balestra, tested O’Dive’s bubble detection capabilities side-by-side with conventional Doppler during a recent DAN field trip i.e., “The APOCALIPTRIP” to the Red Sea in March and came away with positive impressions. “I trust the system for detecting bubbles. It works just fine. Data is still needed of course, and the DAN collaboration will help with that,” he said. A first paper published with Peter Germonpré on recreational Maldivian dives called, “First impressions: use of the Azoth Systems O’Dive subclavian bubble monitor on a liveaboard dive vessel,” will appear in an upcoming issue of Diving and Hyperbaric Medicine. A second paper that addresses technical deep rebreather dives (100m/328 ft) during several days (the Apocaliptrip) comparing O’Dive and echocardiography as bubble detectors will soon be published as well.
When I asked him what he thought about the efficacy of O’Dive’s predictions, Balestra paused for a moment and smiled and offered up his hands. “No one can say it’s wrong. No one can say it’s right. Though given years of development and proper bubble detection, it is unlikely to be totally wrong,” he said.
One thing that people do seem to agree on is that Azoth’s O’Dive has the potential to help educate divers or rather help divers educate themselves.
The Quest to Improve Decompression
O’Dive—the O stands for “optimize”—is the brainchild of Barbaud and research engineer Julien Hugon, who heads the biophysics and computation department at Azoth Systems. The product has been under development for more than a decade.
The original idea for the product dates back to mid-2000s when Barbaud was the officer in charge of diving safety for CEPHISMER—the French equivalent of the US Navy Experimental Diving Unit—and also served as a test diver. At the time, CEPHISMER was developing new decompression tables for Explosives Ordinance Disposal (EOD) divers in conjunction with hyperbaric doctors using Doppler ultrasound and 2D echocardiography technology.
Barbaud was fascinated by the tools and their potential to improve decompression practices. “Given the large number of military dives performed every year, I repeatedly saw people who followed the procedures perfectly and still got bent. It was clear to me that divers needed procedural changes. Not just Navy divers but divers all over the world,” recalled Barbaud, who learned to dive at the Presqu’île de Giens in Southeastern France while at the Naval Academy studying naval operations.

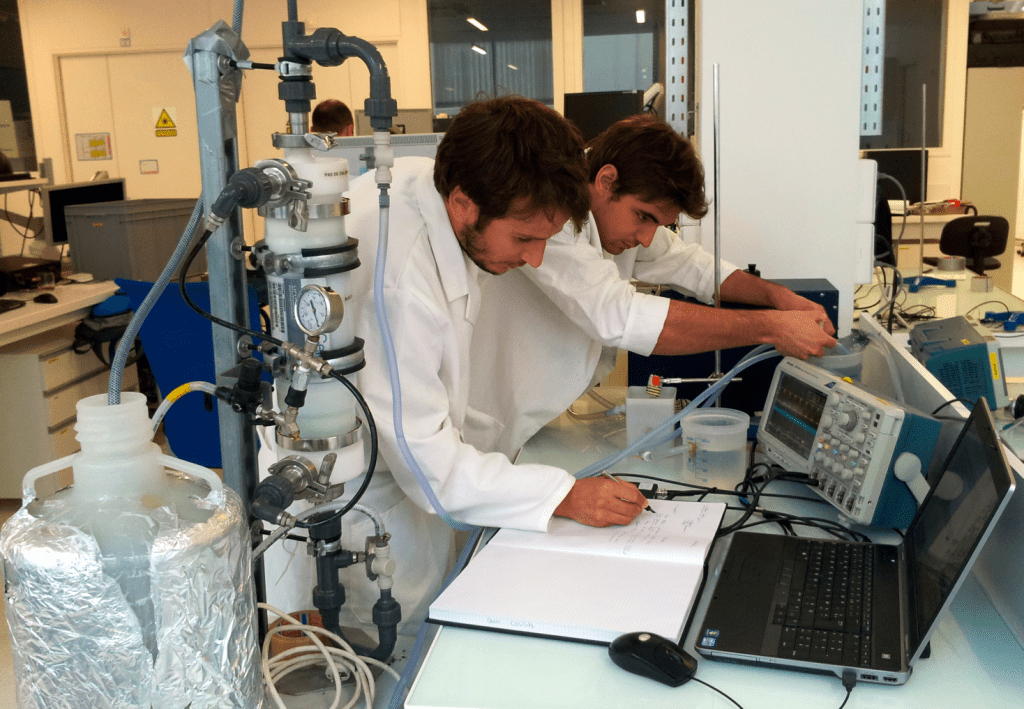
In 2010 Barbaud, then a Commanding Officer of a Naval Amphibious Squadron, decided to take an early retirement from the French Navy to form Bf Systémes in partnership with several labs involved in ultrasound technology and statistical analysis. He was joined by Hugon, who had recently completed his thesis on biophysical decompression modeling using Doppler monitoring.

They soon changed the name of the company to Azoth Systems to better reflect its focus. Azoth is the name of the universal medicine or universal solvent sought in alchemy, while azote is French for nitrogen, to wit: the cure for too much nitrogen? Barbaud was also able to secure grants from the French government to continue Azoth’s research.
The company began by providing consulting services to commercial and military divers, including re-engineering decompression tables using Doppler bubble detection, and began collecting various diving databases for their research. “It was an opportunity to develop a deeper understanding of DCS from an operational viewpoint. I was always thinking about the what-ifs,” Barbaud said. However, their overall goal was to develop a technology that could help divers improve their decompression.
Building an Automated Sensor
Azoth’s initial approach was to focus on precordial Doppler monitoring with the hopes of developing an automated heart sensor. As mentioned above, precordial measurements require a trained ultrasound technician both to place the sensor correctly over the heart in order to get a good reading, and most importantly to interpret the audio signal, i.e., counting the levels of VGE returning to the heart and rendering a score or bubble grade, which requires training and expertise, and good ears due to the complexity of the precordial signal. Take a listen to the difference: Signal 1: Precordial ultrasound without bubbles, Signal 2: Precordial ultrasound with bubbles, Signal 3: Subclavien ultrasound without bubbles, Signal 4: Subclavien ultrasound with bubbles.
Though several scales exist, bubble signals are typically graded on a five-point scale based on the original Spencer Bubble Scale which ranges from 0: No bubble signal, to IV: Bubble signals sounding continuously throughout the systole and diastole and obscuring normal cardiac signals. 2D echocardiography machines, which rely on visual data, use similar but expanded scales.
However, after three years trying to create an automated precordial sensor without success, Barbaud was ready to close the company. Even today, researchers and engineers still haven’t been able to successfully automate the process of grading precordial bubble data.3 As Doppler measurement pioneer Ron Y. Nishi, lead researcher at Canada’s Defence and Civil Institute of Environmental Medicine (DCIEM) explained in a seminal 1993 article titled, “Tiny Bubbles, A Primer on Doppler Bubble Detection,” aquaCORPS #5 BENT“. Although considerable research has been conducted into automatic systems for bubble detection and analysis, none have been successful because of the complexity of the Doppler signal. Bubble identification and classification are still best done by the human brain.”
Instead, Barbaud and Hugon turned their attention to the work of DCIEM, which used post-dive bubble measurements to develop their decompression tables. DCIEM specifically used precordial Doppler, capturing blood returning to the heart in the vena cava; in addition, they took measurements at the left and right subclavian veins (SC) that lie just below the collar bones and bring blood back from the arms, and included these as part of their bubble data.
DCIEM’s use of SC Doppler readings provided the insight that Barbaud and his team were looking for. The audio signal from SC Doppler probe was significantly cleaner and easier to grade than precordial data due to the absence of noise caused by heart valves, which meant that automated grading might be possible. In addition, the collarbone served as a useful reference point to correctly position a probe.
However, a key question for the team was whether measuring SC bubbles provided sufficient information to accurately characterize the level of bubbling in the diver. While precordial measurements capture data on VGE returning to the heart from the entire body, subclavian data only measure VGE returning from the arms. Focusing on that question, they found that subclavian measurements were better statistically correlated with incidents of DCS than Azoth’s precordial measurements, and the correlation improved when the severity of the dive profile was included. They later published their findings in a 2018 paper authored by Hugon, Barbaud, Nishi and others.
As a result, they decided to develop a subclavian Doppler sensor. The plan was to build a device that would be used by divers instead of a medical device built for doctors, which would be subject to government regulation. “I was always thinking of measurement and how divers’ bubbles correlated with the risk of DCS,” Barbaud explained.

By 2015, Azoth Systems had their first prototype, just as the concept of the Internet of Things (IoT)—i.e., Internet-connected devices—was gaining traction. According to Barbaud, the prototype was ugly and not very reliable but it worked. Two years later, they had improved the unit enough to test it with some of their professional diving clients and conduct additional proprietary studies.
As noted above, Azoth officially launched recreational and technical versions of the product at the Paris International Dive Show this year. Each one had its own sensor and associated app.
However, going forward, they have decided to offer a single SC sensor with separate apps for different types of divers: Sport, Advanced, CCR, Technical, and an app for instructors, dive centers, and clubs, enabling divers to share a measurement unit. Azoth will offer existing users an upgrade path. Prices will range from about €530-710 Euros excluding VAT or about US$600-800 before taxes.
Biometrics for Divers
I was intrigued when I opened the waterproof case containing the O’Dive sensor with a wireless charger (with a European power adapter), ultrasound gel, and a compact mirror. I downloaded O’Dive’s Tek app to my iPhone, and set up an account. For a diver who measures and tracks his vitals, heart rate variability, daily activity levels, hiking, swimming workouts, and sleep cycles, the idea of measuring and tracking the quality of my decompressions in the hopes of improving them seemed like an obvious thing to do.

The first step in the process is taking a post-dive Doppler reading. Azoth recommends taking two readings. Each involves taking a 20-second measurement at both the left and right subclavian veins. For helium and rebreather (CCR) dives, they recommend the first reading be taken immediately after the dive, and a second 60 minutes later f. For nitrox and air dives, the readings should be taken 30 minutes after surfacing and then again at 60 minutes post dive. The idea is to catch post-dive VGE levels at their peak.
O’Dive’s smart sensor and app are every bit as sophisticated and user friendly as you would expect from a Garmin or Polar sports tracker, and seem to make the process of obtaining an accurate measurement and bubble grade score easy to do. The app even includes a short built-in demonstration video. You turn on the sensor which pairs with the app via WiFi, and then apply a dab of ultrasound gel to the hockey puck-shaped sensor, which has a groove designed to fit against the collar bone, and a mirror to aid in the placement.
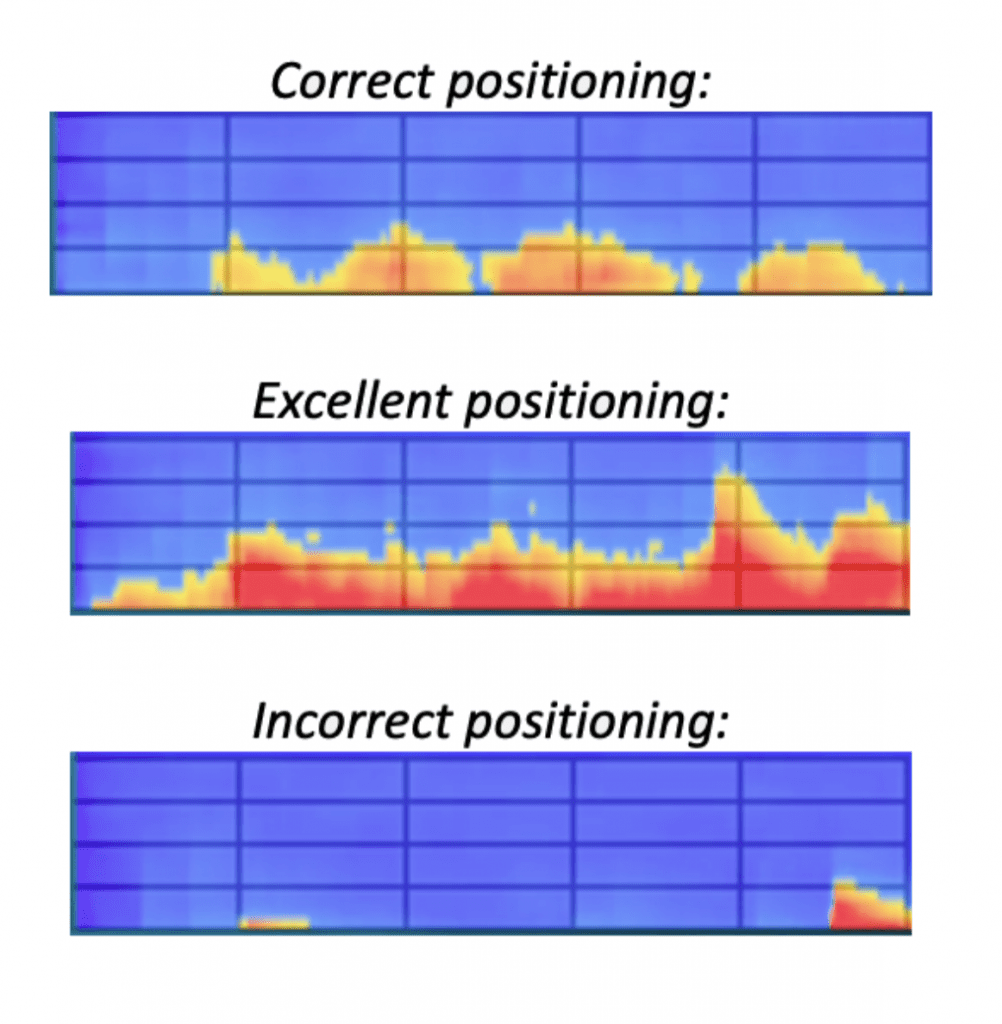
You place the sensor over your left subclavian vein, and the O’Dive app lets you know via the graphic display if the positioning is sufficient to get a good signal. Once the signal is confirmed, you press continue and the app visually directs you to breath in and breath out for 20 seconds while the sensor records the data. When the measurement is completed the app directs you to repeat the process on the right side. It even reminds you when the second post-dive reading needs to be taken.
After taking the two bubble readings, you press synchronize and upload the data along with your dive profile imported from your dive computer or entered manually to the Azoth cloud, hosted in France, via Wi-Fi or a cellular connection. Currently the app communicates with both Shearwater and Suunto dive computers via Bluetooth, and others will likely be added in the future as the number of users grows. Of course, if you are diving in a remote location, your diving data is stored in your device until you have connectivity.
How Good was Your Decompression?

Within a few minutes, depending on your connection, Azoth’s servers perform a comparative statistical analysis of your dive data based on their extensive diving databases. In the process they calculate a decompression quality index (QI) for the dive ranging from 0-100%, which purports to measure the relative safety of the dive from a decompression perspective. The index and associated data are then transmitted back to the user and displayed in the “My Results” section of the app.
The user can now select the dive and see the results in the O’Dive simulation screen, which represents the business end of the unit enabling the user to not only assess their deco quality, but if needed, determine what could be done to improve it. For those who were around in the day, you think of it as crossing the ingenious EDGE tissue saturation graphic with an Excel spreadsheet. “Gee, I wonder how my decompression would look like if my gradient factors were a bit more conservative and I added another 10 minutes of oxygen?” That’s exactly what O’Dive’s predictive model is designed to do.
As shown on the left-hand “Results” side of the simulation graphic, Azoth characterizes a dive with three parameters: the QI, and two components that act to reduce decompression safety. Ideally, divers strive to attain a QI of 100%, which Azoth has benchmarked as the relative risk or probability of DCS of five incidents per 10,000 dives or 0.05%. According to Azoth’s database, this equates to the relative risk of a diver who conducted a no-decompression air dive and has no measured post-dive VGE.
However, as shown, the QI can be reduced by a severity component (Sc), which can vary from 0-100% and represents the relative risk of DCS based on the severity of the dive profile itself in terms of gas loading. This relative risk would be the same for any diver following the specific profile and deco procedures.
The QI can also be reduced by a bubble component (Bc) reflecting the relative risk of DCS based on the diver’s production of bubbles post-dive, which ranges from 0%-40%—the 10% increments i.e., 0%, 10%, 20% etc. theoretically correspond roughly to five bubble grades. Unlike the severity index, the bubble component (Bc) is personal to the diver. Together, the three components, which are mathematically interdependent, add up to 100%. In mathematical terms, QI=1-Sc-Sb.
For decompression management purposes, Azoth segments the QI index into three color-coded “risk” zones which are shown on the left-hand side of the dive quality graphic:
75%-100%: A good quality procedure, where optimization is still possible
50%-75%: Intermediate quality procedure, with significant margin for improvement. Note that a QI lower than 75% is associated in Azoth’s database with a risk higher than two incidents per 1000 or >0.2%
0%-50% The risk is significant and the diver’s procedure needs to be improved. An index lower than 50% is associated with a risk greater than one incident per 100 dives or >1% (the lower bound of the model).
Note that the way that Azoth has scaled their index, every 33% reduction in QI corresponds to a 10-fold increase in risk in the model; in other words, a dive with a QI of 67% is 10x riskier than one with a QI of 100%. Again, Azoth’s intent is to help divers optimize their procedures from one dive to the next.
What If, What Now, What Then
Once the user has gotten their post-dive results, the fun begins. Assuming their QI was less than ideal—okay, it sucked—they can determine what dive factors, if any, could be adjusted to improve their decompression next time around. This is done by adjusting the relevant sliders shown below the dive quality graphic.
The simulated results are then shown in real-time on the right-hand side of the simulation graphic. Geeky divers like me will no doubt find this facility remarkable, though the question remains, how valid is the analysis?
For illustrative purposes, consider a “square” profile air dive to 32 m/105 ft for 56 minutes that a diver conducts using gradient factors of 85/90. More on square profiles later. The diver makes three decompression stops on their “air” back gas: 1 minute at 9m/30ft, 2 minutes at 6m/20ft, and 9 minutes at 3m/10ft. Note, this demo dive profile would NOT be recommended for numerous reasons.
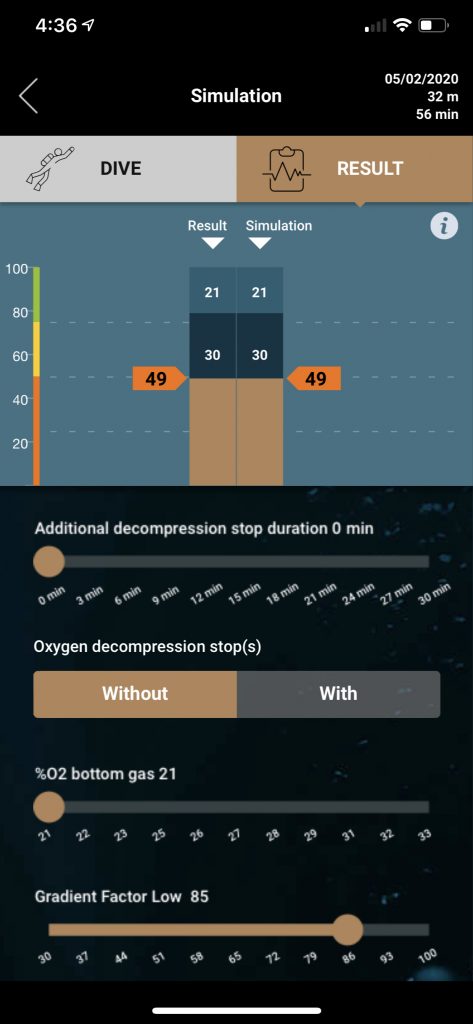
According to O’Dive, the severity (gas loading) component would be 21%, and in this case, the diver has a relatively high bubble grade, which might be expected, resulting in a bubble component of 30%. The resulting QI would be 49%, making it a risky dive with a relative risk of DCS of greater than 1%. What’s to be done?
In the era of nitrox, it’s questionable why the diver would be breathing air in the first place (Reference meme: “Compressed air is for tires.”). Accordingly, the first question to ask is, “What if the diver were breathing nitrox?” The answer can readily be seen immediately by adjusting the slider marked “% O2 bottom gas,” to a standardized 32% mix. Note that the what-if model automatically sets a maximum partial pressure of oxygen (PO2) of 1.4 atm for the working phase of the dive, and a maximum of 1.6 atm for decompression.
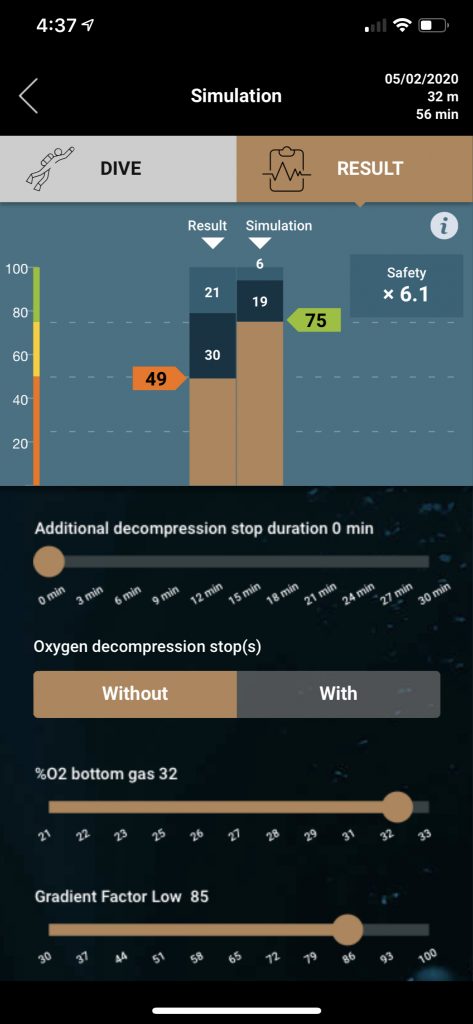
The simulation shows a new QI of 75% along with a severity index of 6% (nitrogen loading is reduced) and a Bubble component of 19%. O’Dive calculates that the diver’s safety has been increased—i.e., the risk of DCS has been decreased—by an estimated 6.1-fold factor, clearly showing the benefits of nitrox. Note that the model has used the new what-if data to predict a reduced bubble grade.
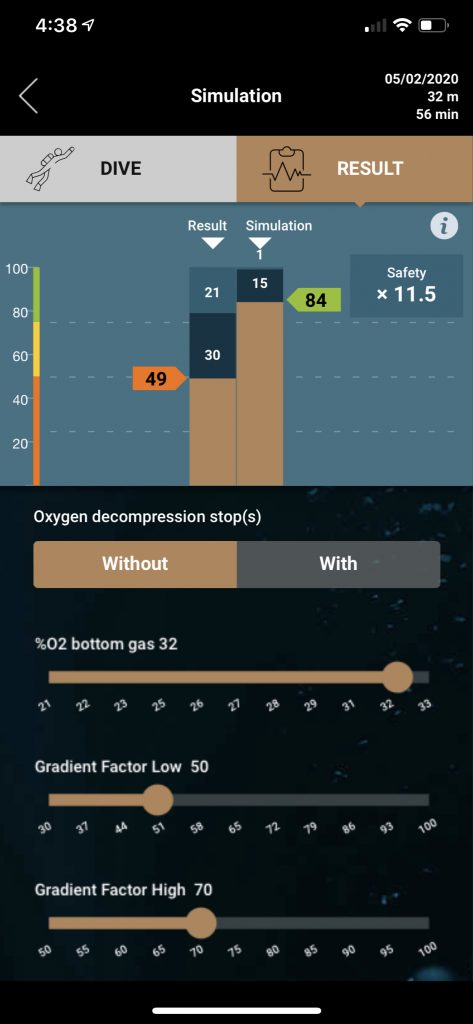
In addition to nitrox, the diver might also consider adjusting their gradient factors (GFs) via the GF Low, and GF High slider. Instead of the current 85/90, what if the diver used GFs of 50/70? Adjusting the sliders, the updated QI index is now 84%, with a severity of 1% and bubble component of 15%, which O’Dive estimates to be 11.5-fold increase in safety over the original dive. Note that the model may limit certain low GF choices, or at least not use them in what-if calculations (the user is notified when this occurs) in order to limit certain “deep stops” which Azoth deems ineffective.
The diver might be satisfied with the results of their decompression at this point. However, they also may consider, “What if they added oxygen decompression?” Usually not a bad thing!
Accordingly, the diver selects the “With Oxygen Decompression Stops” button and moves the “O2 decompression stop %” slider to 100%, which simulates the effect on the dive of breathing O2 on their 6 m/20 ft and 3 m/10 ft stops. After making the adjustments, the model shows that the diver’s QI is now 95%, with 0% severity component and almost zero bubble grade resulting in an estimated 24.2-fold increase in safety over the original decompression.
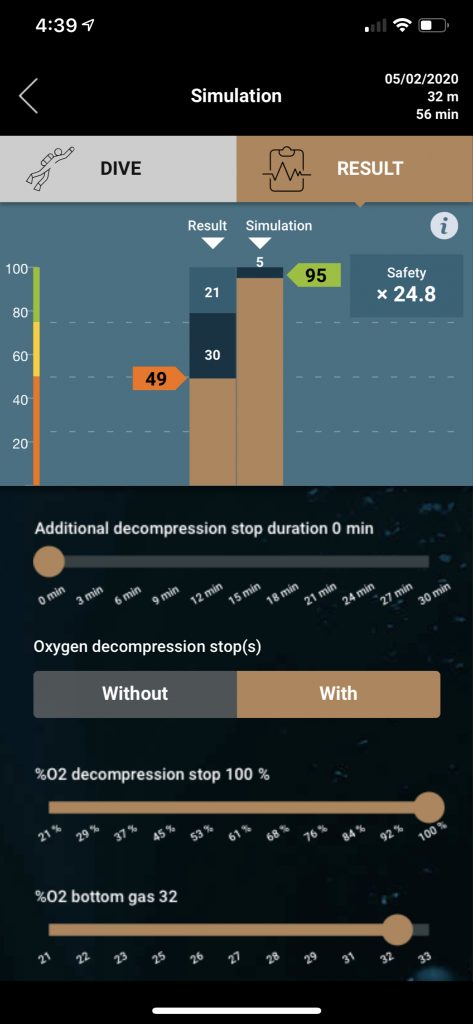
The diver would presumably then make these adjustments to their dive plan, i.e conduct the dive on nitrox 32 with 50/70 gradient factors and use O2 for decompression, on subsequent dives and thus improve their decompression safety. “In the past, people adjusted their gradient factors and other aspects of the dive, in some cases from ridiculous to sane, on what amounted to a wing and a prayer,” observed RAID’s Toomer. “Now they have an actual basis to adjust their procedures.” Providing of course that the predictions proved accurate.
O’Dive performs similar calculations with complex mix or rebreather dives, offering divers the relevant set of adjustments. As noted above, divers can perform what-ifs by adding trimix, adjusting the fractions of helium (FHe) in their bottom mix, adjusting the set point in the case of a CCR dive, adjusting low and high GFs, adding oxygen decompression, adding an additional decompression stop, and/or adjusting the length of the last stop. Note in the case of CCR diving, O’Dive uses the set point, not the diver’s actual PO2. Similarly, the Sport version of the app (designed for no-stop recreational air and nitrox dives) enables the diver to adjust the O2 content in their nitrox mix, change GFs, and add a safety stop of varying length.
It’s easy to be wowed, distracted, or even a bit concerned by the seeming precision of O’Dive’s predictions, i.e., Conducting the dive on nitrox is 6.1 times safer? 6.1?!? Paraphrasing Arthur with a bit of literary license, “This may be some strange usage of the word ‘precision’ that we weren’t previously aware of.” O’Dive’s decimal-place accuracy is a result, primarily of the math, and may be greeted with some skepticism. However the overall idea of presenting divers with an estimate of the “relative risk” of their procedures makes a lot of sense.
Not surprising, Barbaud insists that the apparent precision of Azoth’s algorithms and whether they reflect physiological reality are not the issue. “The QI index is not perfect. The question is does O’Dive help divers to progressively adjust their practice to lower step by step their bubble production?” he proffered to me in an email, and then replied, “The answer, of course, is yes. This can be easily and practically confirmed by everyone using the technology.”
Nevertheless, the fundamental questions remain: how are these calculations made, what do they mean, and how valid are they? For that we take a moderately deep dive into Azoth’s model.
It’s a Math, Math, Math, Math World
I spent considerable time in discussions with Barbaud and Azoth executives trying to understand the logic and mathematics behind their model, and also spoke with several decompression researchers for clarification. (Full disclosure: I have a M.S. degree in Mathematics from Stanford.) Though I don’t pretend to understand the ins and outs well enough to be able to perform the calculations, I came away with a general understanding of the principles behind their work. Here’s what I learned.
In essence, Azoth has worked to mathematically characterize DCS risk based on a number of large databases of dive profiles, to which they have access. Specifically, these are:
• A database of air and nitrogen-oxygen dives in research trials conducted by the United States, United Kingdom and Canadian militaries from 1944 to 1997. This is a collection of more than 8000 exposures and more than 400 DCS cases allowing the analysis of the relationship between diving profile and DCS occurrence.
• Defence Research and Development Canada (DRDC, formerly DCIEM) database that was built from a number of studies conducted by Defence and Civil Institute of Environmental Medicine (DCIEM) over a period of about 40 years. Over 8000 man-exposures that generated 100 DCS have been monitored for bubbles detection and included in this DCIEM/DRDC Doppler ultrasound database. The database includes a large number of open circuit and closed circuit, trimix and heliox dives.
• A subset of French Navy database with more than one million air, nitrox, and trimix dives carried out over the period 2000-2015. The dives recorded in paper format (and do not include dive profiles or ultrasound assessments) have been collected, scanned and checked, including the information of dive parameters and DCS status.
• COMEX Heritage mixed gas diving database which includes a large set of empirical and experimental data on heliox dives shallower than 100 m/330 ft, in addition deeper mixed gas bounce dives.
Having access to large diving databases, characterized by a wide range of DCS risk, has enabled Azoth to make a detailed statistical study of the association between the DCS risk and dive parameters, which they’ve used as the basis of their model. They are not the first. The US Navy, of course, has long used statistical-based algorithms to calculate its decompression schedules, though the algorithms tend to be more complex and consider many more variables.
In contrast to the US Navy’s probabilistic algorithms, Azoth’s predictive model makes a simplifying assumption and only deals with square dive profiles. As a result, when conducting its analysis, Azoth software first converts the dive profile in question into an equivalent square profile. It does this by detecting the start of a diver’s decompression (and speed of ascent), and uses that data to compute an average dive depth and bottom time from leaving the surface. It then proceeds to calculate the risk inherent in the dive profile itself in order to derive the severity Component (Sc) as discussed above.
For air dives, Azoth found that the risk of DCS increases with the depth and the duration of dive, and decreases when the total decompression time increases. Accordingly, Azoth defines a severity index (Is) modified from a formula originally developed by Royal Navy physiologist H.V. Hempleman to measure decompression stress on square profiles as follows:
Is = P √t/dt, where P is the depth in pressure, √t is the square root of bottom time, and dt=total decompression time. As such, Is can be thought of as the ratio between a measure of gas loading and release.
Azoth software then calculates the risk or probability of DCS (pDCS) with the following probabilistic equation: the parameters “a” and “b” are fitted by means of statistical regression analysis using the three defense dive databases.
pDCS=1/(1+exp(-a-b*Is))
The results are shown in the diagram below.
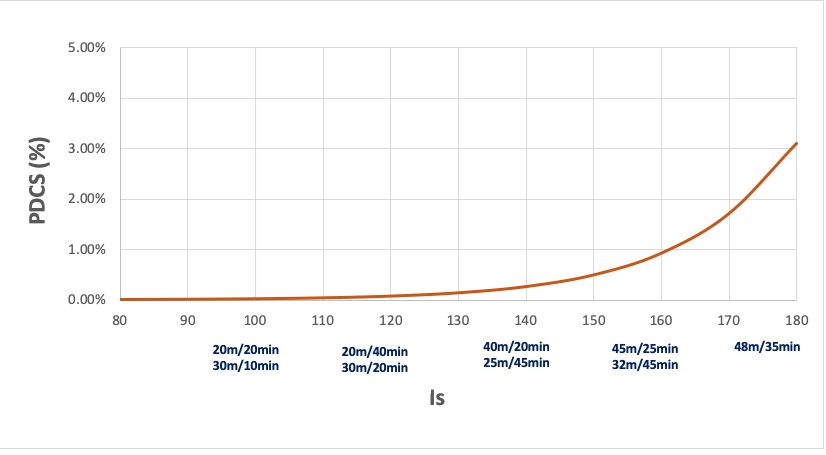
Using the DRDC and COMEX databases, Azoth was able to extend the severity index (Is) to a multi-gas dive, which considers helium mixtures as well the use of nitrox and O2 for decompression. In addition, the Is index is modulated by a coefficient that increases the risk ratio by up to a factor of two, based on the actual ascent rate as compared to the maximum acceptable rate as defined by the COMEX data. This ratio was established indirectly, from a dedicated study on the impact of the ascent rate on the production of bubbles.
More Tiny Bubbles
In Azoth’s world, the presence of measurable venous gas emboli (VGE) circulating in divers’ blood vessels after the dive is an essential element of O’Dive’s risk predictions. Unfortunately, the existence of the VGE has a poor positive predictive value for DCS, meaning that the presence of bubbles doesn’t mean that the diver will suffer DCS. Particularly on the scale of a single dive, the risk ratio of a dive with no bubbles vs. the same dive with many bubbles is unknown, however, according to Azoth, at a scale of many dives the ratio becomes meaningful.
Conversely, VGE has a high negative predictive value for DCS. That is, the risk of DCS is lower in the absence of detectable bubbles. That’s the reason that the O’Dive tool focuses on helping divers to adjust their decompression procedures to progressively lower their bubble scores. Of course, the challenge is that the presence of VGE is the result of numerous physiological factors and is highly variable both between individuals and for a given individual over time.
Nevertheless, based on an analysis of the DRDC database, Azoth theorizes that the presence of bubbles acts an amplifier of risk associated with the severity of the dive profile. In fact, they calculated that the observed risk ratio between a dive without or with few vascular microbubbles and a dive with bubble grade of IV is about 10. Specifically, when the severity of dive profile is considered, Azoth’s model is calibrated so that the DCS risk ratio is close to 2.0x when moving from one bubble grade to the next. The data used in coming to this conclusion is summarized in Table 1.
| Grade SC | N observations | % | N DCS | % DCS |
| 0 | 665 | 61.3 % | 4 | 0.6 % |
| 1 | 163 | 15 % | 3 | 1.8 % |
| 2 | 104 | 9.6 % | 2 | 1.9 % |
| 3 | 140 | 12.0 % | 11 | 7.9 % |
| 4 | 13 | 1.2 % | 3 | 23.1 % |
| Total | 1085 | 100 % | 23 | 2.1 % |
Combining their severity index and bubble grade, Azoth calculates the risk or probability of DCS (pDCS) by means of statistical regression analysis, where again, the parameters a, b, and c, are fit to the data. The resulting risk curves are shown in Figure 8.
pDCS=1/(1+exp(-a-b*Is-c*Grade))
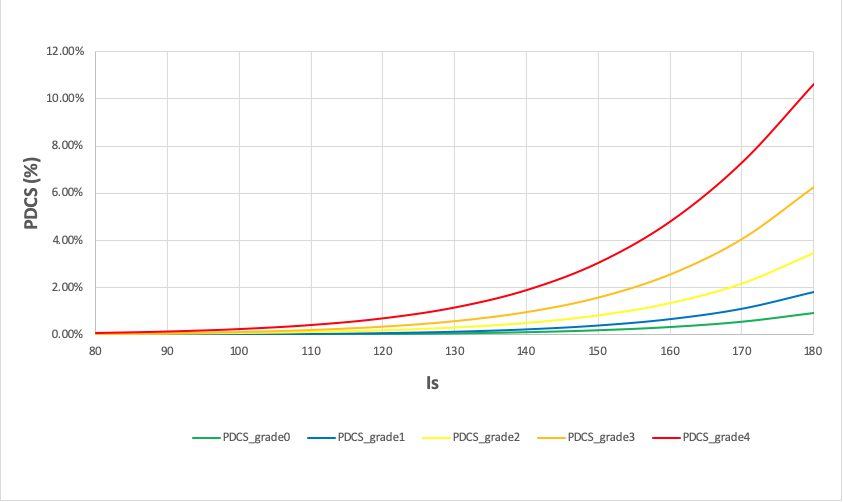
Note that O’Dive’s use of subclavian bubble data, which offers a much cleaner signal than precordial Doppler, enables Azoth cloud software to essentially count the number of bubbles in the diver’s post-dive readings using spectral analysis, thus automating the scoring process. The software then converts the highest measurement to a five-point bubble grade scale, similar to the Spencer scale, used in the equations above. As noted above, this potentially represents a significant breakthrough in Doppler monitoring, insofar as accurate measurements can be made by the diver themselves. No small feat.
Once the diver’s profile, including decompression procedures, and bubble scores are uploaded, Azoth software calculates the QI decompression quality index, which now can be understood as the logarithm of a product of risk ratios, specifically the risk of the dive in question from a severity perspective compared to Azoth’s baseline no-decompression air dive, amplified by the diver’s bubble grade. This enables the index QI to be expressed as a sum of probabilities. In mathematical terms:
QI=
MAX (1-0.33*LOG{[PDCS(Is)/PDCS(Is_Air_NoD_limit)] *[PDCS(Grade, Is)/
PDCS(Grade=0,Is)]}
Equivalently:
QI=1-Sc-Bc where Bc=.1*Bubble Grade
and Sc= MIN(0.33*LOG{[PDCS(Is)/PDCS(Is_Air_NoD_limit)];1-Bc).
In addition to the QI, the software also calculates various risk ratios between the risk of the underlying dive in question, and the risk of the dive when relevant what-if factors are activated. For example, using the above case of the air dive to 32 m/105 ft for 56 minutes, the software calculates the range of risk of the same profile if it had been conducted on a range of nitrox mixtures i.e., air (21%) through nitrox 33 (at which point the PO2=1.4, the maximum permitted for bottom mix by the model). These ratios are then transmitted to the diver’s device along with the QI and other relevant data, enabling the user to perform what-if calculations locally on their device.
As noted above, O’Dive’s model also predicts the diver’s bubble grade for the simulated what-if dive. In fact, the model progressively adapts its predictions based on diver’s past bubble history, which it characterizes into one of three classes of diver bubbling dynamics: low, medium, or high, identified through the DRDC database. Think of it as a kind of moving average based on the diver’s history.
Researchers have long known that some individuals, so-called “bubblers,” consistently bubble while others rarely do. Azoth argues that one of the strengths of O’Dive is that it actually takes the individual’s history into account, offering a personalized what-if.
“Again, do the sliders reflect the perfect reality of gas effects on every diver in the world?” Barbaud asked me rhetorically in an email in response to my questions. “Of course not!” he answered. “Nor are they built on pure supposition with no basis at all. The truth is in between these two positions; they are not perfect BUT they reflect a good reality,” he wrote. “They are simulations of the next dive, and provide indications that are more accurate than pure intuition, a supposition-based idea or no idea at all. This approach was designed to help divers reduce their bubble production and consequently improve their practice.”
Barbaud compared the situation to the first introduction of the dive computers. “Can we say that dive computers brought perfect information to divers? No. But they did bring a huge step forward to diving practice!” Did I mention that Barbaud and team are swinging for the bleachers?
What Works, Works?
As might be expected with a product as intriguing and complex as O’Dive, the diving and hyperbaric medicine scientists I queried had plenty to say about Azoth’s approach and procedures. Decompression physiologist David Doolette who is intimately familiar with the US Navy’s statistical approach to decompression raised several issues about Azoth’s model itself. The first question out of his mouth when we spoke? “How do they validate any of this mathematically?” Azoth’s answer: The model has been tested against the DRDC, French Navy, and COMEX Heritage databases from which they were derived.
One of Doolette’s concerns about Azoth’s model was that it treats post-dive venous gas emboli (VGE) as an input to the model and not an output. “They have VGE on the wrong side of the equation,“ he explained. ”The problem is that the VGE measurement doesn’t really cause DCS, it’s a parallel or surrogate outcome to DCS that is closely related to the dive profile and consequently Azoth’s severity index (Is).” Note that the model predicts future VGE based on the severity index and current VGE. The result according to Doolette is that there is collinearity in the model which could make it unstable and lead to poor predictions in the field. “If the model worked, it would be great. But I question whether it’s ready for primetime,” Doolette said. Two other researchers shared his assessment.

“If this were a [peer-reviewed] scientific paper I would ask them to show me an external calibration set such as DAN Europe’s DSL dataset or DAN US’s Project Dive Exploration and see if they could predict it,” he said. Azoth has or is about to enter into a collaborative agreement with DAN Europe, so it’s possible that may come about. Currently the company does not have access to either of DAN’s diving databases.
For his part, Barbaud respectfully acknowledged the limitations of VGE, but questioned the physiologist’s premise. “There is room for being imperfect, while still adding interesting value. The fact that the information contained in bubble grades and dive profiles is not the same is reflected by the significant improvement in both the likelihood and the information criteria when bubble grades data is added to the dive profile DCS model. This prevents it from being unstable,” he said. However, this does not address Doolette’s concern with the accuracy of O’Dive’s predictions with new data.
To his credit, Barbaud said that Azoth is always open to suggestions for improvement. “If someone can prove there’s a better way to do it, we’ll listen. We are focused on improving safety and enhancing our tool. That’s what counts.”
A final question for Doolette: Whatever its accuracy, could O’Dive’s predictive algorithm actually make a diver who wasn’t trying to abuse the model less safe? “No, I don’t think so,” he said. “Assuming all the equations I have not seen are correct.”
JP Imbert, a French diving engineer involved with designing decompression procedures for the offshore industry suggests a larger view of the issue. Imbert has worked with Hugon in the past, and was the lead author of a recent scientific paper with Balestra and others that offers a new model on bubble formation. “There is more to decompression safety than just bubbles. We have measured an oxidative stress after deep and long saturation decompressions in the commercial diving world. Inflammation could be the second dimension of the decompression stress, he explained. ”Inflammation is related in the scientific literature to free radicals and microparticles but we do not know yet if there is a link between microparticles and VGE. High oxygen levels and pre-existing microbubbles could be responsible for it.”

DAN’s Tillmans also had questions about the model. While impressed with O’Dive’s sensor, which she called “ingenious,“ Tillmans pointed out that decompression stress encompasses many factors besides bubbles including temperature, age, sex, sleep, BMI, and more. “A lot of science is ignored by only considering time, depth, gradient factors, and bubbles,” she said. “I believe Azoth has done everything they possibly could do, but I don’t think it’s the full-scale picture. They may prove me wrong.”
Barbaud acknowledged her points while at the same time pointing out the associated research challenges. “Yes, we know bubbles are not all there are. There are a lot of factors like sleep, temperature, activity levels, and others. But how do we take these into consideration? What is good sleep, or bad sleep and how do you quantify this? Wait for 20 years and try to count the number of DCS in various situations? No. Instead, we can compare various situations in terms of bubble production. Our goal is to educate divers to lower their bubble scores dive after dive, which we know can only increase their safety.”
In the Field
Another issue raised by scientists who have spent time conducting field research is that Azoth’s bubble measurement protocol of taking only two measurements is inadequate to reliably capture peak bubble data, i.e., the reading with the highest bubble grade. As Pollock, who has been using ultrasonic monitoring to evaluate decompression risk for more than three decades, explained, “The goal of course is to catch the bubble peak, but taking only two measures will almost certainly miss it in some cases. The consensus recommendation of the ultrasound workshop conference was that a minimum sampling of every 20 minutes for two hours is required to achieve research quality data,” he explained.
“If self-monitoring misses peak bubble scores the predictions would be fundamentally flawed, and it is clear that the time to peak grade can vary. Collecting high quality data is often not convenient or easy,” Pollock said. In the case of trying to catch peak bubbles, more data is better. In addition, field researchers typically measure subjects both at rest and after doing knee bends or arm flexes.

Barbaud said that Azoth’s two measurement protocol was determined based on the observation of their databases. “If the diver properly follows these time slots, they will catch the peak in 90% of the time we will not miss the bubble peak,” he said and referred me to DAN’s APOCALIPTRIP trip data that showed a good correspondence between O’Dive’s and Balestra’s echocardiographic readings.
Barbaud also noted that the system was not developed for a single use, but rather was designed to adapt progressively to a user’s practice over three to five dives. “We may miss the bubble peak on a single dive but not every dive, and so the global trend for the diver (in terms of bubbling dynamic) will quickly appear. Regarding the knee bend and arm flexes, we know these practices very well of course. But we’ve observed in our databases that DCS is better correlated to bubble peaks at rest than after an exertion. What’s more, it doesn’t require any specific action from the diver, which is welcome if we want our product to be widely used,” Barbaud said.

One of the questions surrounding Azoth is what they will do with the volume of diver data that are accumulating from users, and whether it will be helpful to further decompression research. O’Dive users will of course have access to their diving data including their bubble scores much in the way they do now with their Shearwater computer via the Shearwater cloud app. Presumably, the data will help Azoth to improve their model and Barbaud said that they would also make the data available to legitimate researchers.
However, on the question of whether the data will be useful for decompression research, the scientists I spoke to were not encouraging.
The first issue is that of the quality of the data as discussed above, which may be impacted by Azoth’s protocols, as well as the uncontrolled nature of the data collection. “The ability of a monitor to closely track a professional precordial monitor under controlled conditions is very different from a device able to monitor effectively under dynamic conditions, and still interpret the findings in a meaningful way,” Pollock said.
The second issue is the same problem inherent in the two DAN dive profile databases. According to Doolette, “Lots of ‘safe’ data doesn’t tell you much and can become a data management nightmare,” he said. “You can’t pick and choose which bits you look at either, because you lose the bulk probability context. You do not, for instance, learn anything by choosing a subset that resulted in DCS and say 50% of these dives had high VGE. Maybe 50% of all dives had high VGE.”
Feed Your Head

Given those caveats and possible limitations, almost everyone I spoke to agreed that O’Dive had the potential of being a powerful learning tool for divers, if only to measure how their own bodies respond to their diving practice. As discussed above, the ability for divers to now self-monitor their post-dive VGE is arguably a significant breakthrough in its own right.
I reached out to Stockdale, who has been working with colleagues and testing the product under a variety of conditions including cold water exposures, to get his perspective. “I can understand why the medical professionals are freaked out,” he said. “Many of them are passionate divers themselves, and they worry that divers could misuse the product, like seeing how far they could push the limits before getting bent. Ever since Doolette and [Simon] Mitchell’s 2013 paper on deep stops, everyone has become a deco theory expert,” he chuckled.
Stockdale’s take on the product? “I think O’Dive is an effective education tool for divers to help them understand what works for them, and also for instructors who are teaching divers about decompression principles. I think that’s where its strengths are. It could also be a powerful tool for specialists like researchers and hyperbaric docs, and expedition divers. It’s the biggest game changer since mixed gas dive computers,” he said.
His outlook was seconded by IANTD’s Heylen. “Even for a basic diver, it’s a great tool to become more aware of the realities of diving; not just the false belief that nothing can happen to you. It will help them increase their knowledge, and get divers interested in knowing more.” Arguably, education can only be good for diving safety!
Like the introduction of dive computers to sport diving, it will likely take time, additional studies and more experience to determine whether O’Dive is the next EDGE, more akin to first analog dive computer, the SOS Automatic Decompression Meter, affectionately known as “The Bendomatic,” introduced by the Torino, Italy-based company Strumenti Ottici Subacquei in 1959, or somewhere in between. The ultimate test, as Barbaud and team have proffered, will be whether O’Dive is able to actually improve divers’ safety.

In the meantime, divers are advised to remember that like dive computers that came before it, O’Dive’s models should be taken for what they are, mathematical representations of what we perceive as reality. It’s a message that Pollock has been delivering in his talks and papers for many years. “Developing new tools is important, particularly those that can be used by divers in their own practice. But it’s crucial for users to understand the limitations of any device to avoid confusing the information they provide with truth,” Pollock said. “While O’Dive may prove useful helping divers consider their options, we still have a long way to go in both physiological monitoring and data analysis to truly assess personal risk.”
Azoth System’s O’Dive is arguably a bold and innovative new step in that direction.
Footnotes:
1. Note that the Divetronic AG DecoBrain, which was introduced the same year in Europe, was a table-based look-up decompression meter.
2. Scientific diving may have the lowest incident rate of the various diving communities.
3. There have been some promising developments in recent years using portable 2D echocardiography and frame-based bubble counting.
Dive Deeper
NETVA 2012 interview Axel Barbaud – BF Systèmes (En Francais)
La France bouge : Axel Barbaud, fondateur d’Azoth Systems January, 2020
Additional Papers
Carturan D, Boussuges P, Vanuxem P, Bar-hen A, Burnet H, Gardette B. Ascent rate, age, maximal oxygen uptake, adiposity, and circulating venous bubbles after diving. J App Physiol. 1999; 93: 1349-1356.
Pollock NW. Use of ultrasound in decompression research 2007: Diving Hyperb Med. 2007: 37(2):68-72
Dardeau MR, Pollock NW, McDonald CM, Lang MA. The incidence rate of decompression illness in 10 years of scientific diving. Diving Hyperb Med. 2012; 42(4): 195-200.
Balestra C, Germonpre P. The use of portable 2D echocardiography and ‘frame-based’ bubble counting as a tool to evaluate diving decompression stress. Diving Hyperb Med. 2014: 44(1):5-13
Møllerløkken A, Blogg SL, Doolette DJ, Nishi RY, Pollock NW. Consensus guidelines for the use of ultrasound for diving research. Diving Hyperb Med. 2016; 46(1): 26-32.
Doolette DJ. Venous gas emboli detected by two-dimensional echocardiography are an imperfect surrogate endpoint for decompression sickness. Diving Hyperb Med. 2016: 46(1): 4-10
Papadopoulou V et al. Variability in circulating gas emboli after a same scuba diving exposure. Eur J Appl Physiol, 2018. 118(6): p. 1255-1264.
Hugon J, Metelkina A, Barbaud A, Nishi R, Bouak F, Blatteau JE et Gempp E, Reliability of venous gas embolism detection in the subclavian area for decompression stress assessment following scuba diving. Diving Hyperb Med. 2018 Sep; 48(3): 132–140.
Imbert JP, Egi SM, Germonpre P, Balestra C. “Static metabolic bubbles as precursors of vascular gas emboli during divers’ decompression: a hypothesis explaining bubbling variability,” Front. Physiol., 11 July 2019
Balestra C, et al., Diving physiopathology: the end of certainties? Food for thought. Minerva Anestesiol, 2019. 85(10): 1129-1137.
Menduno M. It’s the metabolism, stupid: a new model for bubble formation. DAN Europe’s Alert Diver 2020