Diving Medicine
Is Animal Testing Still Needed in Diving Medicine?
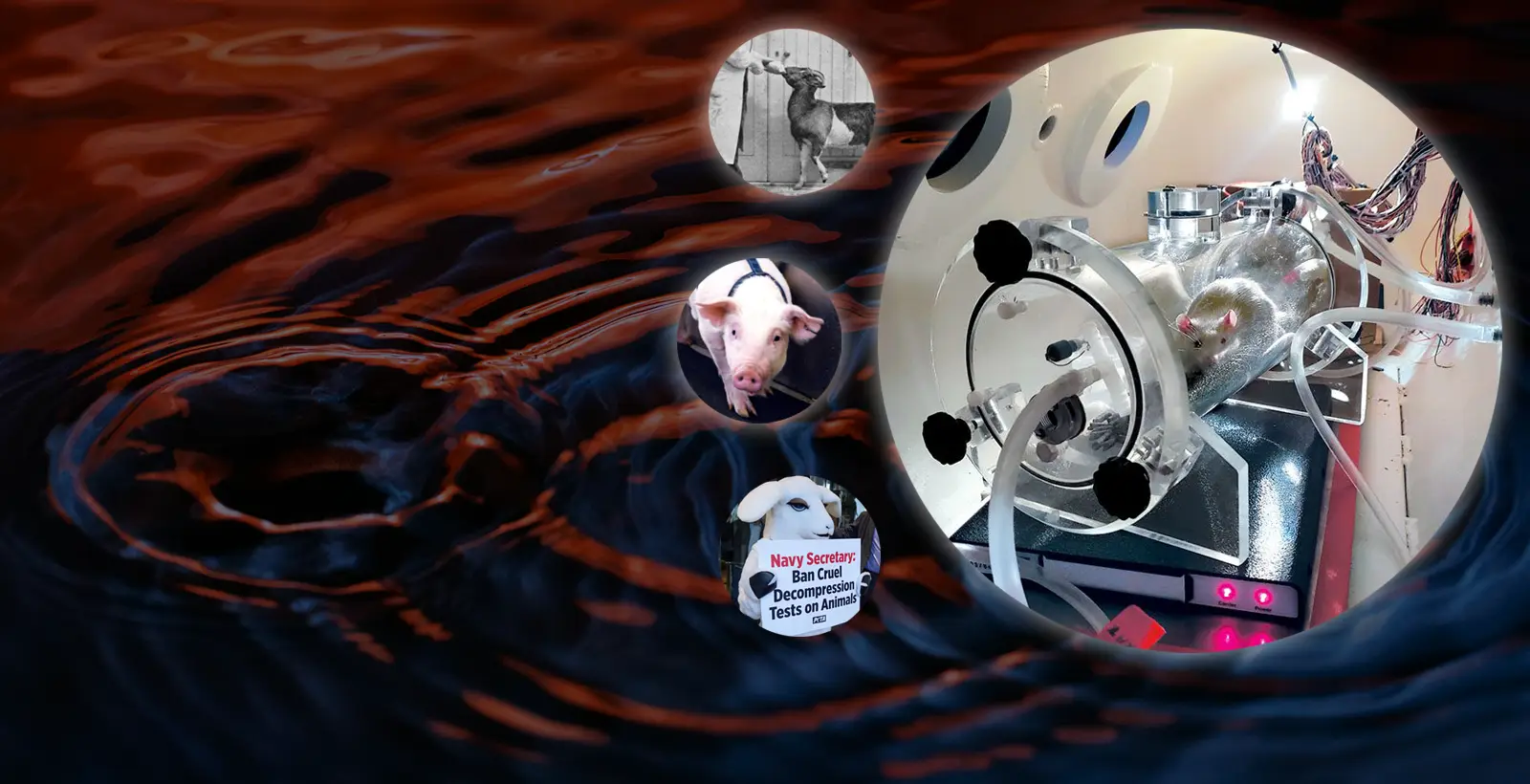
Historically, much of what we know about decompression and oxygen toxicity has been the result of animal research. Today however, animal rights activists want to shut down the practice claiming that it is unethical, cruel and ineffective. Diving journalist Mark Cowan reviews the history and efficacy of animal testing and speaks with the scientists at the front line, who argue that animal research is critical for developing treatments and preventions needed to protect divers and submariners who put themselves in harm’s way.
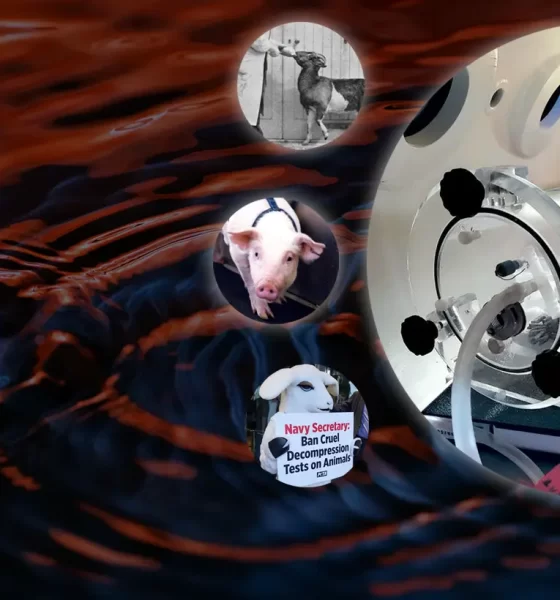
by Mark Cowan. Lead image: Collage by Rico Besserdich. Photos courtesy of the author and PETA unless noted.
Every time you surface safely from a dive, you owe a debt to a goat, or a sheep, a dog, a baboon, rat, or mouse. Why? Because in the long history of our chosen pastime, a lab animal has suffered a bend or a seizure, maybe even died, during an experiment in the ongoing quest for the perfect decompression protocol.
You’ve not seen these tests, maybe not even heard or read about them, even as you benefit from them. Typically, they look something like this: an animal is placed inside a pressure chamber and taken on a simulated dive. Sometimes, they are fitted with sensors to measure signals from the body or brain or cannulas to take blood or administer drugs. Sometimes, they are made to trot on a treadmill. Sometimes, they develop decompression sickness. Sometimes, they experience a seizure from oxygen poisoning. And sometimes, they are euthanized at the end of the experiment so an animal autopsy can be conducted to examine their injuries.
Animal testing is a reality of diving medicine: something we as divers must own. It poses an ethical dilemma that is perhaps incomprehensible to anyone outside the field of science—one that researchers bear with nothing more than the goal of improving divers’ safety underwater and saving lives.
It has been that way ever since 1878, when French physiologist Paul Bert first suggested that the mystery malady affecting divers, miners, and bridge builders might have something to do with nitrogen bubbles.
Today, more than 130 years after Bert’s studies, animal testing is still being conducted in the name of diving medicine. The issue remains controversial and divisive. Animal rights advocates have called on the US Navy to end funding animal experiments, claiming they are an inhumane and ineffective way to investigate problems when progress could be made using new technologies.
Scientists involved in diving medicine reject those claims, arguing that animal research remains critical for developing treatments and preventions to protect divers and submariners who put themselves in harm’s way on behalf of national security.
What We Know About DCS
Ask any scientist in the field of diving medicine how much we know about what causes the bends, and their answer will often be something to the effect of, “Not very much.” At one time, the prevailing thought was that decompression sickness was solely about bubbles. Today, in part due to extensive research, there is an emerging theory that DCS might also have something to do with a diver’s immune system.
The US Navy spends millions of dollars each year supporting researchers across the country who are trying to determine the exact causes of decompression illness and oxygen toxicity and to identify potential mitigations—countermeasures in military speak—to overcome them.
That such efforts continue might surprise many divers who generally put their faith in the well-worn research running real-time computations inside the devices on their wrists to keep them safe.
Decompression sickness affects a vanishingly small number of divers, between 0.01 and 0.1 percent per dive, depending on the type of dive. But people still get bent. A 2017 DAN Europe Research Division study examined 39,000 dives and 320 cases of DCS. In almost all those cases, divers with DCS had not strayed from the “currently adopted safety limits” of their respective algorithms and were ascending with compartment inert gas pressures well below the maxima allowed. In other words, they got the bends while following the accepted rules.
“Despite knowing about decompression sickness for more than 300 years, we still do not know enough to cure it or prevent it with certainty,” said Dr. Sandra Chapman, PhD.
Dr. Chapman is the program manager of the Undersea Medicine program at the Office of Naval Research, the department that funds much of the current research into DCS and oxygen toxicity at research institutions across the US.

“Our understanding of DCS is still built on assumptions that may not fully capture the precise etiology of the disease. While models provide generally acceptable guidance for diving safely, diving is not without risk due to the inherent nature of relying on probabilistic models, and it comes with strict limitations to depth and time that dictate dive profiles.”
Dive tables and decompression algorithms, then, are good enough to get the overwhelming majority of divers safely to the surface. For the Navy, being good enough is not necessarily good enough. In military terms, being just good enough doesn’t win fights. We have to do better.
Today, decompression sickness and oxygen toxicity remain the two most significant factors that limit how long and deep military divers can go. “Limitations” is not a welcome word in military circles. Extending time and depth parameters for divers propels much of the current research supported by the ONR.
Extending no-decompression limits to give military divers a greater margin to operate in is one thing. The holy grail of the program, Dr. Chapman said, was to understand the biological mechanisms responsible for DCS “so we can develop a targeted treatment, or ideally a preventative prophylactic.”

Military rebreather diver. Photo courtesy of JFD.
A drug to prevent the bends? Science fiction? Maybe. To make that breakthrough, scientists are going beyond the theoretical that has driven diving medicine in the past. They are now focusing significant resources on pinpointing what happens to the body at a cellular level—particularly the immune system’s response to decompression stress—during and after dives.
“When looking for a reliable cure or preventative measure, it’s important to fully understand what is happening at the molecular, cellular, and tissue level during the progression of the disease,” said Dr. Chapman.
“We know bubbles do not equal DCS; therefore, our current indicator is flawed. So, we need to identify a specific biomarker with a high correlative association with disease onset and the precise bad-acting agents associated with DCS. A better understanding of what immune cells drive symptoms could lead to drugs that prevent their activation.”
Developments in diving medicine are a slow, methodical, step-by-step process, Dr. Chapman acknowledged. “We hope that currently funded research will identify potential ways to lessen DCS risk that can be investigated in the future.”
Animal Testing and Diving Medicine Today
In scientific circles, the conventional wisdom is that the study of specific cells in the body can be performed using tissue cultures and cellular models. For those trying to answer complex systemic questions, like the uptake of inert gases in tissues throughout the body, or disease progression involving dynamic interactions across multiple organs, the only way is to study a living system. That means testing on animals.
Testing on animals plays a significant role in biomedical research into a wide range of diseases—from cancer and diabetes to neurodegenerative conditions like dementia and Parkinson’s—testing that would be unethical, morally unacceptable, or too difficult to perform on humans. According to the Foundation for Biomedical Research, 95 percent of all lab animals used in medical research are rats and mice. Researchers study rats and mice because their bodies work similarly to human functions.
Rodents are widely used in diving medicine, as well. Researchers at the University of Maryland, for instance, are using mice in a $981,996 study to investigate the role of microparticles shed from cells in glymphatic dysfunction and neuroinflammation during exposure to high-pressure gas. The study has already found that decompression stress could cause a systemic inflammatory process—including prolonged neuroinflammation—and it aims to assess the potential for pharmaceuticals to offset injuries to the central nervous system.
At the University of South Florida, mice and rats have been used in various experiments searching for ways of predicting and mitigating CNS oxygen toxicity (CNS-OT). These studies, funded by Navy grants of more than $3 million, have:
- Explored whether a ketone ester supplement could delay the onset of seizures
- Identified the possibility of significantly increasing the time Navy rebreather divers can spend at depth
- Identified a biomarker—an increase in lab rats’ breathing rates—that could predict the onset of seizures by several minutes and lead to the creation of a mask-fitted respiration rate monitoring device
- Investigated the possibility of using a mitochondria-targeted antioxidant therapy to delay or prevent CNS-OT
The researchers are currently trying to locate oxygen-sensitive neurons that trigger seizures.
Meanwhile, furthering the pursuit of DCS origins, researchers at the University of California San Diego used rats in novel experiments to track gas uptake through the body during a simulated dive. The research team exposed the rats to a breathing mix containing radioactive nitrogen-13 gas. Then, they used a positron emission tomography scanner to measure the concentration of the gas as it moved around the animal’s body.
An examination of the organs post-dive showed substantially elevated radiation levels above background levels in all subjects. The brain, thigh muscle, and femur bone had lower radiation counts than the blood and liver. The findings of the study, funded by a Navy grant of $1 million, offer a potential breakthrough in identifying the pathways of inert gases during dive conditions and provide another step toward understanding the processes of decompression sickness.
Physiologist and Duke University associate professor of anesthesiology Heath Gasier, PhD, uses mice as part of a new wave of research to find a prophylactic countermeasure to offset the effects of CNS-OT.

Research has shown that high levels of oxygen cause oxidative tissue injury at a cellular level, damaging mitochondria that produce energy necessary for cell function. Damaged cells are removed in the hours and days after tissue injury, and new mitochondria are formed. Studies have shown that oxidant brain injury and mitochondria turnover can be reduced by an antiepileptic drug that increases the amount of a neurotransmitter known as gamma-aminobutyric acid (GABA) in the brain. However, the problem scientists face is that a second exposure to hyperbaric oxygen up to ten days later can interrupt this process and exacerbate the severity of the original injury.
In September 2022, the Office of Naval Research awarded Dr. Gasier a three-year $844,714 grant to study the use of the drug and determine whether he could get it to work over multiple exposures. Dr. Gasier acknowledged that what happened in the brain at a molecular level still needed to be correctly understood. “If you want to find safe mitigation strategies, you have to understand the pathology.”

The first step for him is to understand further what happens in the brain during mitochondrial turnover after exposure to high oxygen levels. To answer those questions, Dr. Gasier conducts tests using mice because they are similar to humans in their sensitivity to oxygen exposure. During tests, mice are exposed to oxygen at 4.5 ATA for 60 minutes. During a single exposure, 80 percent of mice developed seizures. When mice are administered the antiepileptic drug, the number that develop seizures is almost halved. Follow-up tests are conducted between 48 hours and seven days later. Samples of brain tissues are then taken and subjected to chemical analysis to understand how the drug influences sensitivity to tissue injury in repeated exposures.
Dr. Gasier is aware of the ethical concerns about testing on animals – “In another lifetime, I would have been a veterinarian,” he said, but there currently exists no alternative to getting the answers he needs. “If I could bypass this, it would be wonderful, but we don’t yet fully understand the human body. This is where it starts. To be part of really helping humanity, you have to accept that animal research is a part of that.”

Pigs and sheep, meanwhile, have been used to evaluate the Navy’s protocol for rescuing submariners from a partially flooded vessel disabled on a seabed. In the event of a submarine accident, the US Navy deploys the Submarine Rescue Diving and Recompression System (SRDRS) to recover stranded submariners. The SRDRS is a remotely operated vehicle that can recover 16 personnel at a time and decompress them back to the surface. According to SRDRS, rescue is possible for submariners trapped in a partially flooded submarine at an internal pressure of up to 5 ATA, or 40 m/132 ft of seawater. However, the time taken to decompress each group means the last crew members to be rescued could remain at 5 ATA for up to 172 hours.
The Naval Medical Research Center in Silver Springs, Maryland, used pigs in experiments to measure the risks posed by the rescue protocol after such a prolonged stay under pressure. During the experiments, pigs were placed in a chamber and exposed to high pressure for a week while breathing elevated levels of carbon dioxide. The pigs were then decompressed to the surface and monitored. None survived beyond 55 hours.
The research highlighted concerns that increased levels of carbon dioxide in rescued submariners could exacerbate symptoms of pulmonary oxygen toxicity and could increase injuries and death associated with decompression sickness.
Follow-up studies, funded with $775,000 from the Naval Sea Systems Command, were carried out at the University of Wisconsin School of Medicine and Public Health using sheep. The findings provided fresh input to DISSUB rescue planning and execution and to determine the inherent risks associated with prolonged time under pressure.
When it came to testing on animals, now-retired Navy physiologist Dr. Susan Kayar said researchers understood the duty of care they had to their animals.
In the 1990s, Dr. Kayar was hired by the Naval Medical Research Institute (NMRI) as a physiologist for their experimental hydrogen diving program. At the time, the Navy was looking at the feasibility of using hydrogen instead of helium as a diluent gas for extreme deep dives.

One part of her project was to look at something the NMRI had called “biochemical decompression”, placing hydrogenase enzymes inside the intestines to consume hydrogen gas and reduce decompression times. If the theory worked, the enzymes would work like a biological scrubber inside the body, eating the hydrogen gas and producing methane. This methane would be released from the intestines on ascent every time a diver passed wind. The diver would, in effect, fart their way to shorter hang times.
Kayar first conducted tests on male Sprague-Dawley rats before moving on to pigs. Animals got bent during the tests. The signs of decompression sickness were primarily neurological, and those diagnosed were euthanized inside the chamber.

“When it was time to say goodbye to the pig, we did it as quickly and kindly as we could,” she said. “These animals were sentient creatures, and we didn’t want to be cruel to them. We had to treat them humanely. I didn’t wish to do any harm to my pigs. I had compassion for the animals I worked with, but I also had compassion for navy divers. There was a higher goal.”
A Brief History of Animal Testing
Scientists have been testing on animals for almost as long as divers have been suffering the effects of decompression sickness.
In the 1870s, French physiologist Paul Bert—arguably the first to systematically investigate the effects of changing pressure on high-altitude ballooners, caisson workers, and divers—conducted tests using sparrows, rats, rabbits, cats, and dogs.

Bert’s experiments numbered about 670, and he detailed many in his book, La Pression Barométrique, published in 1878. Take, for instance, experiment DXXVIII conducted on a small dog. On June 18, 1875, the dog was bound to an iron frame inside a cylindrical steel pressure chamber under the pressure of ten atmospheres. After an hour, Bert cranked open a valve and let the air spill out of the chamber in three minutes. The effects of sudden decompression were startling. “There are no other movements than respiration,” Bert wrote. “Constant cries of pain.”
The dog died shortly afterward. During the autopsy, Bert observed the right side of the heart and the veins were full of gas, and the dog’s blood had turned to foam. An analysis found the bubbles contained nitrogen.

Two decades later, when John Scott Haldane was appointed to the Admiralty Committee on Deep Diving to consider how Royal Navy men could “dive safely and do valuable work” in thirty fathoms (55 m/180 ft), he tested his theories on goats. Goats were chosen because they were large enough to show “plenty of symptoms of inappropriate decompression.”

In the summer of 1906, Haldane’s team at the Lister Institute of Preventive Medicine in London exposed goats to the strain of decompression. At the end of each trial, the animals were released into the yard, and their handlers kept careful watch for anything untoward. Symptoms typically appeared in the first 30 minutes; however, one of the smaller, thinner goats was prostrate very quickly. The creatures stood in the yard, one lame leg held aloft, or staggered about, hind legs strung out behind them. Collapsed in the hay, they turned up their noses at corn and gnawed at their paralyzed limbs. Labored breathing was a precursor to death. Some succumbed in five or ten minutes; others lasted thirty. Three survived for 40 hours.
Post-mortem examinations revealed the white matter of the animals’ spinal cords was frothed with bubbles, and tissues had already started to soften.
The results of the animal experiments provided Haldane with sufficient information to test his theories on Navy divers. The two decompression tables he created revolutionized diving at the time; problems with decompression sickness in Royal Navy divers vanished almost overnight.

Two decades later, researchers again turned to animals when the Admiralty asked for diving tables that could send a man deeper than before and use oxygen to accelerate decompression. They established a colony at Siebe Gorman & Co.’s Neptune Works in London. Pigs and dogs were quickly deemed unduly susceptible to compressed air illness, while the baboons were immune, so researchers again prioritized results from their experiments with goats. They were a sacrifice deemed necessary by the Navy to get workable tables that could get men safely down to 91 m/300 ft and back again.
Ethical Improvements in Modern Animal Testing
Over the years, much has changed about the approach to animal testing, mainly when it concerns oversight.
Dr. Heath Gasier from Duke University said that many legal checks and balances were now in place to ensure ethical treatment of animals. He said, “You can’t just say, ‘I’m going to do this [animal test]’ like they used to … I don’t think I would have been able to do animal research the way they did. Today, there are many hurdles, and rightfully so.”

At a federal level, the Animal Welfare Act and the Public Health Service Policy on Humane Care and Use of Laboratory Animals set standards of care for laboratory animals in housing, feeding, cleanliness, the use of anesthesia, and post-operative care.
Research institutions using animals are also required by law to establish an Institutional Animal Care and Use Committee (IACUC) to oversee the work. The IACUCs require researchers to submit detailed proposals justifying the need for animal testing. Researchers must declare all aspects of their experiments, including the potential harm to an animal, how they plan to address that harm, how they plan to reduce pain to an animal, and what protocols they have in place should something unplanned happen to threaten an animal’s life.
“The committees learn and change,” said one researcher previously involved in animal studies. “What was being looked for in reviews 10 or 15 years ago differs from what’s being looked at now. The group doing the review considers everything; their job is to assess the harm-benefit analysis. Is there a potential benefit to the study? What are the potential harms to the animals?’’
The Fight Against Animal Trials
Given the moral and ethical objections concerning animal testing, it was inevitable that animal rights advocates would raise concerns about the treatment of animals by scientists and universities engaged in Navy-funded research.

People for the Ethical Treatment of Animals (PETA) believe that animal experiments are ethically inexcusable. For the last 15 years, PETA has been running a campaign calling on the Navy to end funding for such research. The organization has written letters to Navy officials, and activists dressed as sheep have attended naval and defense conferences in protest. More than 100 Navy veterans recently co-signed a letter calling for a ban on all tests.
As far as PETA is concerned, there is “no scientific legal or ethical justification” for subjecting animals to tests. The tests, they claim, are gruesome, cruel, and ineffectual, subject a variety of species to the possibility of prolonged pain and suffering, including paralysis and death, and the group denies such tests help produce new drugs.
PETA’s Science Policy Officers have scoured research documents to highlight testing methods they consider “inhumane”. They have examined official investigations into events where animals have died unexpectedly before or during experiments due to equipment failure. They have condemned tests that have induced decompression sickness or oxygen-induced seizures in animals.
“The management and treatment of decompression sickness and oxygen toxicity hasn’t changed for years,” said Shriya Swaminathan, Science Policy Officer for PETA. “We’re not seeing anything significant come out of this.
“Given the anatomical and physiological differences between these animals and humans, we are wasting taxpayers’ funds on experiments that are harmful to animals and have failed to provide human-relevant data.
“Animals are not ours to experiment on. Their lives carry an inherent worth. They shouldn’t be bred into existence just to be used, experimented on, and killed.”

The ethical question about testing on animals is not lost on researchers. Eric Sandgren, Professor of Experimental Pathology at the University of Wisconsin-Madison, who was involved in US Navy-funded animal testing, said, “I think it’s ethical to use animals under certain conditions if it’s an important enough problem and if the animals are well cared for.
“Some people think of animals as family members, and even if we could learn something important by studying and potentially hurting animals, they’d say no.
“I respect that perspective, just as I’d expect them to respect mine. It is an issue of values. It’s not that they’re wrong; they have a very different value system. I believe the benefits to people outweigh the potential harms.”
Others accuse activists of targeting scientists and institutions conducting legally allowed research with name-and-shame campaigns. For them, they choose to say nothing and keep their head down. “You wait for it to go away,” one researcher said. “Most of what was written was erroneous, but it is what it is.”
Sometimes, though, researchers can’t keep their heads down low enough.
In 2010, nine members of a research team at the University of Wisconsin-Madison found themselves named in a criminal investigation after animal rights advocates petitioned a court to bring animal cruelty charges against them over experiments involving the decompression of sheep.
The researchers, funded by a grant under the Navy’s Deep Submergence Biomedical Program, were studying the physiological effects of decompression on submariners during rescue.

As part of the study, sheep were placed in a hyperbaric chamber pressurized to the equivalent of 27m/90 ft for 24 hours, decompressed, and monitored for signs of decompression sickness. Ultimately, each animal was euthanized, and a necropsy (animal autopsy) was conducted to examine the effects of decompression on the sheep.
Under the testing protocol, if during an experiment, an animal appeared in distress, researchers had to remove it from the chamber and administer drugs to euthanize it. In three years, three animals died of complications before being euthanized. When PETA and the Wisconsin-based Alliance for Animals found out about the deaths, they called on the local District Attorney to act. When he refused, they petitioned a judge, arguing the deaths broke an obscure Wisconsin law that prohibited killing an animal through decompression. The judge appointed a special prosecutor to investigate the claims.
As far as the university was concerned, no laws had been broken, and the studies had provided valuable information to the Navy; one of the reported findings concerned the onset of osteoporosis, which might occur through continual deep diving.
Prof Sandgren, who was the director of UW-Madison’s Research Animals Resources Center at the time, said, “We had to stop the study until everything could be sorted out. People were thinking they could go to jail. I don’t know how likely that was, but that was scary for people.”
Ultimately, the special prosecutor dismissed the claims against the scientists. He determined the law, while ambiguous, had originally been introduced to prevent the mass euthanasia of unwanted cats and dogs and did not apply to those engaged in scientific research.
By then, the special prosecutor’s report didn’t matter; the Navy had pulled the grant, and the project stopped. Prof Sandgren said the legal case left a bitter taste. “You couldn’t say it didn’t [have a chilling effect on research] because we had to stop. It was unfortunate because the Navy was getting some interesting information.”
Novel Animal Testing Alternatives
With current advances in modern technology and the growing possibilities of artificial intelligence, PETA says that testing on animals should now be obsolete.
“We would like to see the Navy championing human-relevant methods,” said the group’s Science Policy Officer, Shyria Swaminathan. “We’re seeing so many technological advancements in this space. We can only envision how much farther along we would be if instead of wasting taxpayer dollars on animal-based experiments that are not human-relevant, we develop these technological advancements: the organ-on-a-chip models, the computational models, the in vitro studies using human tissues.”
In recent years, scientists have harnessed technological advances to aid the study of decompression sickness and oxygen toxicity. Researchers in Slovakia used human cell cultures derived from human fibroblasts and cell cultures of mice neuroblasts to examine what happened at a cellular and subcellular level during decompression. In Bergen, Norway, scientists used human umbilical vein endothelial cells to investigate whether nitric oxide in the body offered protection against bubble formation and the risk of decompression sickness.
The Office of Naval Research has funded and continues to invest in studies using non-animal technology. Investigators in Pennsylvania, and now at Ohio State, have conducted in vitro diving simulations using human dermal fibroblast cells to examine cellular stress and what happens to mitochondrial function during dives.
In a $500,000 Navy-funded project at the University of Colorado Boulder, scientists are using a physiologically relevant human lung-on-a-chip model to mimic how gas moves through the lungs. The chip is seeded with human lung microvascular endothelial cells on one side and human pulmonary artery endothelial cells on the other. The team used the chip to investigate whether dissolved gas contributes to the activation of immune cells under increased ambient pressure. Findings from the study are a step toward identifying biomarkers in divers that could trigger the body’s immune response and cause DCS.
Meanwhile, researchers at the University of Maryland School of Medicine have used blood samples from divers diagnosed with decompression sickness to examine the presence of micro-particles and inflammatory proteins. The study has added further evidence to the theory that diving triggers an inflammatory response in the body. It also found a reduction in plasma gelsolin, a protein that mediates the immune response. Researchers now want to see if an infusion of plasma gelsolin could help control inflammatory events in divers.

Elsewhere, studies have used human diver data to fine-tune decompression models. Throughout the 1980s and 1990s, researchers at the US Navy, including Drs. P.K. Weathersby, Lou Homer, Ed Flynn, Ed Thalmann developed decompression modeling using a powerful statistical approach called the maximum likelihood principle. Instead of specifying critical thresholds for decompression tables, the researchers used the principle to investigate the benefits of a probabilistic approach to designing decompression tables. Their early work was informed by diver data from the US, UK, and Canadian navies. At the same time, the Navy Experimental Diving Unit and Cdr. Thalmann developed and tested non-probabilistic, real-time algorithms in early dive computers used by Navy rebreather divers.
Dr. Bruce Wienke was also a pioneer in the field of dive-specific algorithm design and routinely analyzed data banks to tweak models to better predict decompression risk factors in diving. Meanwhile, researchers at the DAN Europe’s Research Division used a database of electronically recorded recreational open circuit dives to examine the quality of decompression algorithms. They concluded that the algorithms were good at predicting the decompression risk in fast tissues but were “potentially deficient” in identifying the correct gradient factor in medium tissues.
While emerging technologies provide new opportunities for scientists, the National Association of Biomedical Research says animal studies remain necessary because human biological systems are incredibly complex and still not fully understood. Artificial intelligence, meanwhile, remains far off.
“If we fully understood mammalian physiology at the molecular level, then research would be data-driven,” added Dr. Gasier from Duke University, “but we don’t; we’re not there yet.”
The US Navy said it “shares the goal” of replacing animal models with alternative models. In a written response to PETA’s campaign, the Secretary of the Navy, Carlos Del Toro, stated the Navy looked to refine, reduce, and replace animal use whenever practical. In the meantime, he added the Navy would prioritize the ethical treatment of animals used in research.
While the debate continues, retired Navy physiologist Susan Kayar said no one should lose sight of exactly who researchers were ultimately looking to protect. “Navy divers don’t have a choice about whether they dive,” said Kayar. “They do incredible work for the Navy, and it’s not fair to leave them dangling, wondering if they will bend. And if they bend, can we do something to look after them? If you’re asking them to push to the limit, you have a duty of care to them.”
Along those lines, when you next go diving, spare a thought Tarzan and Pongo, two baboons among dozens of animals enrolled in the dive testing program at Neptune Works factory belonging to Siebe Gorman & Co., in Lambeth.
In the summer of 1930, they were designated test subjects in a series of studies by renowned physiologist Leonard Hill. His goal was to examine the use of oxygen to accelerate decompression and identify the dangers of oxygen toxicity.
Before Hill asked any human diver to breathe pure oxygen under pressure, he took Tarzan and Pongo on a series of chamber dives beneath 91m/300 ft. The tests provided “sufficient information” to draw up a new set of decompression tables for human use, and a dozen divers volunteered to test them in Scotland.
Tarzan and Pongo were the first primates to reach 122m/400 ft; no volunteer diver was tested at that depth during the Admiralty program. Later, it was determined the pair was remarkably immune from decompression sickness and oxygen toxicity.
And that was that. The baboons were retired from the program, and no further record was made of them. However, their lives are a reminder of how humans have used animals in pursuit of our ambitions to make it safely into the deep and back again.
DIVE DEEPER
InDEPTH: Imagineering The Future of Diving by Rachel Lance
InDEPTH: Meet the D-Day Scientists That Operationalized Self-contained Diving by Rachel Lance
Alert Diver: Deep in the science of diving: The Navy Experimental Diving Unit.
Other Stories by Mark:
InDEPTH: He’s Got The Power: Meet Tech’s 22-year old Go-To DPV Guy by Mark Cowan
InDEPTH: Peter Readey’s Incredible Steam Machine by Mark Cowan
InDEPTH: Between the Devil and the Deep and the DCS—My Own by Mark Cowan

Mark Cowan is a journalist with over two decades’ experience in newspapers and television. He spent twelve years on the police beat covering the war on crime for a series of newspapers in Birmingham, UK, and reported on the peace-keeping operations in war-torn Kosovo while embedded with the British Army. He has worked on a number of documentaries, including the BAFTA-winning Gun Number 6 which was inspired by his original reporting on the realities of gun crime in the UK. He has been a diver for 20 years, is a PADI Master Scuba Diver Trainer, trained to use a rebreather in 2012, and learned to cave dive while researching and writing the book Between the Devil and the Deep, One Man’s Battle to Beat the Bends with co-author Martin Robson. He is an avid wreck diver and is now based in Chicago, Illinois.