Latest Features
DCS is on the Rise Amongst Freedivers
Divers tend to think of decompression sickness (DCS) as an affliction of compressed gas diving, but as scuba instructor turned freediver Charly Stringer reports, free divers not only suffer from DCS, but the incident rate also appears to be on the rise. Not surprising, given that freedivers are collectively pushing their underwater envelope to great effect. Here’s what’s happening and how the community may want to deal with it. In-water recompression anyone?
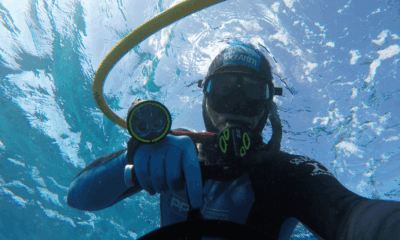
By Charly Stringer. Lead image: an athlete breathing O2 at 5m after a 100m deep training dive at Freediving World, Sharm El-Sheikh. Photo courtesy of Denys Rylov.
Contrary to popular belief, decompression sickness (DCS) is not just a risk for scubies and techies. While, for freedivers, the risk is not as high, the fact that we know very little about the causes of DCS in freediving makes it a conversation we need to continue having. Leveraging the years of research we have on DCS in scuba diving, we can try to apply our knowledge to the freediving world to reduce freedivers’ risks as much as possible.
I spoke to some important voices in the medical freediving world to explore what we currently do know about DCS in freediving and what the future might look like for deep freedivers who want to avoid getting bent. We will also discuss the slightly taboo topic of freedivers who choose to take recompression into their own hands.
DCS in freediving is known in the medical community as Taravana syndrome: “This syndrome is characterized by the onset of neurological symptoms after deep or repeated dives. The main clinical manifestations are cerebral, including stroke and cognitive impairment. The pathophysiology of Taravana syndrome is still widely debated, but the most accepted theory is that it is a specific form of decompression sickness” (Druelle et al., 2024).
Although DAN’s research tells us that DCS in freediving is much rarer than in scuba or tech: “Freedivers simply do not on-gas enough nitrogen to provoke DCS,” Taravana has definitely become a more prevalent issue in freediving in the last few years. This is likely attributable to the general rise in freediving’s popularity; more divers means more people reaching for deeper depths. And the idea of “deep” has massively evolved during the past 30 years.
In 1994, the absolute world record was roughly 70 m/230 ft deep; today it stands at over 135 m/443 ft. That’s a huge jump in only three decades. With the “100 Meter Club” gaining more and more members, it’s no longer an achievement made by a small handful of super elite divers—it’s seen as much more achievable (yet still very impressive; don’t get me wrong). There are also better freediving setups and easier access to facilities around the world making deeper dives easier to organize.
Dr. Juani Valdivia, freediver and neurosurgeon, told me that, as a doctor who is very involved in the freediving community, he has definitely seen more cases arise of late: “I have personally been involved in at least two cases of DCS in freediving myself (in person), and at least five other cases remotely where I’ve given assessment and guidance from a distance.” So, it seems the problem is likely to get worse before it gets better; if that’s the case, what can we do?

Who Is At Risk Of Getting DCS In Freediving?
Decompression sickness (DCS) in diving is a medical condition caused by the absorption of inert gas at depth followed by inadequate decompression. DCS is a condition that falls under the blanket of decompression illness (DCI), which includes both DCS and arterial gas embolism (AGE). The terms are sometimes used interchangeably, and they’re also sometimes more casually known as “getting bent.” Signs and symptoms of DCS include fatigue, joint pain, shortness of breath, and confusion, just to name a few; if left untreated, it can be fatal.
Divers who breathe compressed air are at a higher risk of experiencing DCS due to longer bottom times, but they can also plan for avoiding DCS by reducing dive times, having long surface intervals, and surfacing slowly. Scientists have conducted years of research related to avoiding DCS in scuba diving but, in freediving, it is a relatively new and unexplored issue. And, in freediving, we simply don’t have the same rules and guidelines in place to follow to avoid it.
All we really know is that freedivers might experience Taravana if they dive very deep, make multiple deep dives back-to-back, have fast dive times, or don’t leave a long enough surface interval gap in between their dives: “These diving habits increase tissue nitrogen loading during descent and bottom time and decrease nitrogen unloading during ascent and surface time, leading to the formation of bubbles” (Druelle et al., 2024).
But, taking a look at recent cases of Taravana, it seems like it can hit a freediver rather unpredictably. For example, divers might do a training stint of multiple deep dives without incident, take a long rest period, come back, and suffer DCS on their first deep dive back in the water. So, is it possible to pinpoint who is more at risk of Taravana, and why?

Unfortunately, we still don’t have enough research into many aspects of health and safety in freediving, not least around DCS. At the moment, the best we can do is extrapolate from available scuba research around risk factors for DCS—scuba research has had a huge head start. I asked Marta Marrocco, Senior Case Manager at DAN Europe, whether the statistics tell us if sex plays a part in one’s risk of getting bent. She told me, “Statistically speaking, I can confirm that we report in proportion more DCI or suspected DCI cases in women compared to men. While our insured members are 70% men and 30% women, the DCI/suspected DCI cases that we record are 60% men and 40% women. Nevertheless, we have also learned that these numbers are also to be taken with the perspective that, generally speaking, women tend to be more self-conscious or insecure about their bodies compared to men; they tend to report that they are sick or that they have some symptoms, while men might not.”
Despite this anecdotal (qualitative) evidence, there is no concrete statistical or scientific (quantitative) evidence that women are more susceptible to DCI. Dr. Valdivia said on the matter: “To my knowledge, there haven’t been any reported cases of Taravana in female freedivers so far.” The scuba research does tell us that age can play a part, though. Dr. Valdivia summed this up for me: “The older you are, the more at-risk of DCS you are, potentially just due to general lower health and fitness or preexisting conditions that might come with age.” DAN tells us that the following can also increase a diver’s risk of DCS (Thalmann):
- Poor health and fitness
- Obesity
- Dehydration
- Heart disease
But, DAN also noted that, “Some divers get DCS more frequently than others despite following the same dive profile.”
Currently, these variables are not clear in freediving specifically, and there is not enough data to support that these factors are just as relevant for freediving as they are for scuba. Dr. Valdivia confirmed this, adding, “There haven’t been studies on all the freedivers who have had DCS, and some of the cases haven’t reported their DCS. Taravana can be underreported, just as respiratory barotrauma of freediving can be, too, perhaps due to the stigma that comes with having a ‘hit,’ or perhaps due to pressure to perform competitively.”
Dr. Valdivia suggests, though, that having a patent foramen ovale (PFO) could put a freediver at a higher risk of Taravana: “If we had to generalize and say what are the two most possible causes, I would say: 1. Having a PFO (which causes an air bubble to go from the right chamber to the left chamber in the heart). 2. Intrapulmonary shunt (blood passes through the lungs but fails to take part in gas exchange).”
This 2021 study regarding the risk of DCS with a right-to-left shunt (RLS), (Germonpré et al., 2021) backs this up. The results show that, “DCS is more frequent in divers with RLS (such as a PFO).” However, it also states, “It appears this risk is linked to diving behavior, more specifically diving to the limits of the adopted decompression procedures.”
There is no way to fully predict who might suffer from DCS in freediving. Dr. Valdivia suggested that the focus should be not only on finding more whys and hows, but also on lowering the risk as much as we can based on what we do know. For example:
- Depth: Dives deeper than 100 m/330 ft increase the risk of Taravana, according to the literature.
- Multiple dives with short surface intervals: E.g., Multiple dives to just 20-30 m/30-100 ft with short breaks in between have also been reported as a cause of Taravana. High rate of ascent can also play a part (just like it does in scuba).
- Dehydration: This is something that should always be on our minds as freedivers. We tend to be in the water, and the Dive Reflex has diuretic (water loss) effects that can dehydrate you without symptoms.
- Pre-existing medical issues: Conditions like diabetes, heart disease, or a PFO can make your chances of getting DCS much higher.
- Distal arterial bubble (Arieli): A decompression bubble that can form in a distal artery, and is thought to be a cause of neurological disorders in breath-hold divers and (DCS).
Freedivers should always consider these risk factors.

How Freedivers Can More Effectively Combat DCS
The main thing we can control in regards to avoiding DCS in freediving is our reaction times. Part of a freediving safety’s job is to look out for signs of trouble even after their buddy surfaces. Dr. Valdivia says that it’s imperative to continue this vigilance even long after their dive is complete.
“DCS can manifest immediately upon surfacing, or even for a long while afterwards, so we always need to be observing and asking the diver how they are doing and feeling, he said. “I think this is a huge habit that should be implemented in the freediving industry more often by the community: Ask how your buddy is doing 15, 20, even 30 minutes after their deep dive.”
Dr. Valdivia identified an issue back in 2016 while taking an International Association for the Development of Apnea (AIDA) freediving instructor course in the remote area of Dominica. He recognized that many freediving hubs and training spots are in remote locations with no access to a decompression chamber and with scarce medical facilities. Using his expertise in the field, he decided to create a tool that every freediver can use: an acronym to follow to help keep their buddies safe. He has kindly explained this acronym to me, with a hope that more and more freedivers will start to use it as a standard: M.F.S.C.O.2 (he suggests that any certified Freediver can remember this easily with the freediving-related words: MouthFill, Snorkel, CO2. OR: Mask, Fins, Snorkel, CO2). This is what the acronym really stands for:
M: Memory and motor skills
F: Feeling and fine motor skills
S: Speech
C: Coordination
O: Orientation
2: Two eyes (eye exam)
Using this tool, you can perform your own neurological exam anywhere in the world, without the need of a doctor, a medical professional on site, or a laminated neuro exam guide that may be cumbersome. By progressing through each letter, you can monitor a freediver in the 30 minute window following their deep dive, catch neurological deficits quickly, and trigger a fast evacuation response if needed. Dr. Valdivia told me, “The sooner someone gets medical attention for a neurological issue such as DCS, the better the outcome.” He continued, “The only concrete thing we know about DCS in freediving is that a diver experiencing it needs to be evacuated to a chamber as soon as possible. This is what you should always be prepared for.”
Questions you can ask someone with suspected Taravana include:
- “How are you feeling?”
- “Do you have any memory issues?”
- “Can you walk ok?”
- “How is your balance?” and
- “Is your vision normal?” among others.
Questions like these are simple, but they are crucial for early detection of DCS. Dr. Valdivia added, “These checks should be done at the platform or boat; don’t wait until you are back at shore two hours later. This would be a good habit to cultivate within the community.”
Standard freediving protocol should also include the following: Before a training session, locate the nearest chamber; know the evacuation route to the chamber, have the procedure on standby, and trigger that procedure quickly when you suspect DCS.

Should Freedivers Be Reentering The Water To Recompress?
Following a competition dive or record attempt, it is not uncommon to see freedivers breathing from a tank of pure O2 while holding onto a dive line at around 5 m/16 ft deep [Ed. note: Freedivers seemed to have standardized around 5m/16 ft not 6m/20 ft like tech divers]. Some freedivers choose to do this for a few minutes after their deep dive for the same reason scuba divers do a safety stop; it allows you to off-gas before exiting the water while still under some pressure. It’s a “prophylactic” to reduce the risk of getting bent.
However, it has been reported that some deep freedivers who have experienced symptoms of DCS after a dive have re-entered the water with an oxygen tank in an attempt to recompress themselves and alleviate the Taravana. This is known as in-water recompression (IWR) and is, of course, a fairly risky decision especially without the supervision of a medical professional. However, it could be a faster way to treat Taravana if the diver is in a very remote location.
Regarding the prophylactic approach (not to be confused with IWR for someone already experiencing DCS symptoms), opinions around breathing O2 to “recompress” vary within the freediving community. Some are all for it, whereas others do not advocate the method citing the risks of O2 lung toxicity nervous system O2 toxicity. The latter puts the diver at risk of seizures underwater (if they were to breathe pure O2 deeper than 5m/16 ft underwater, for example). [Ed. note: The tech community regards 6m/20 ft, i.e., PO2=1.6 ATM as the maximum for O2 breathing, though oxygen toxicity convulsions have occurred at PO2=1.4]
Dr. Valdivia told me, “There’s no evidence in the literature we currently have to advocate for either side regarding prophylactic recompression after deep dives. All we know is that this is current practice by a percentage of deep freedivers…whether the scientific community or the scuba community approves or not.” Although this is not an uncommon practice in the tech world, it simply hasn’t been studied enough for freediving and it is not taught as part of the curriculum. It is being practiced with zero rules or guidelines; freedivers might even be doing this alone with no prior knowledge or experience of scuba diving, potentially going too deep to do it safely.
Dr. Valdivia continued to suggest ways to make the process safer when a freediver chooses this approach: “One cannot advocate on what to do, but rather on what not to do, in order to minimize risk. This includes: Making sure no one is breathing pure O2 deeper than five meters and making sure that no one is recompressing alone in this way. This is crucial. If you are alone, breathing 100% O2 at depth, you do stand the risk of developing oxygen toxicity which leads to a seizure and underwater loss of consciousness. If this happens when you are alone underwater, the inevitable can happen.”
Regarding IWR for Taravana, Dr. Valdivia adds, “Even though I have been physician for more than a handful of cases with successful improvement after IWR, with complete resolution of neurological deficits in remote areas, the general consensus currently in the freediving community and freediving agencies/industry is to avoid IWR and, rather, prioritize the gold standard: surface oxygen, hydration, and prompt transfer to hyperbaric chamber.” This is simply because there is not enough research and, therefore, there are no official guidelines in place yet.
In a 2019 InDepth article, “A New Look at In-Water Recompression (IWR),” Reilly Fogarty explored the subject of IWR within the world of technical diving: “What if you are more than two hours from a chamber? If you are prepared (that means having the right equipment, training, and know-how), the new consensus among the hyperbaric docs is to treat with In-Water Recompression” (Fogarty, 2019). The article explains that opinions on IWR in the tech diving world mirror those in the freediving world: “Depending on who you ask, in-water recompression (IWR) is either a critical life-saving tool for experienced divers or a fast-track to becoming a case report.”
Now, I think most will agree with Reilly: “Putting a diver back in the water after a serious injury is not something to be taken lightly. Managing the diver requires significant training and equipment, as well as the training to diagnose a diver before treatment and manage them and any possible complications afterwards.” But, if you are hours from a hyperbaric chamber and experience life-threatening symptoms, is it not worth trying something that could save your life—or at least buy you more time? Dr. Valdivia added, on this point, that anyone using IWR should use caution: “IWR has to be considered treatment and, as in any surgery, treatment can cause harm.”
Although technical diving and freediving are very different activities, DCS is DCS, and the symptoms are the same regardless of how it came about, right? So, the same treatment can be applied. A 2018 article, “In-water Recompression” in Diving and Hyperbaric Medicine explains that IWR is “no more beneficial” than conventional first aid, surface oxygen, and transport to the nearest chamber. However, the benefit is that it can be done immediately: “In military training and experimental diving, delay to recompression is typically less than two hours and more than 90% of cases have complete resolution of manifestations during the first treatment, often within minutes of recompression” (Doolette and Mitchell, 2018).
But, there is a real risk that you could exit the water in a worse condition or not exit the water at all. A major risk of IWR is that of an oxygen convulsion resulting in drowning.
If a freediver is performing a dive that could pose DCS risks and chooses not to do in-water recompression, all they can do is monitor themselves for any signs of Taravana after the dive, ensure they have a proper emergency action plan that includes an evacuation plan, and have freediving buddies with training to recognize signs of DCS who are ready to take action.
InDEPTH plans to delve into the subject of IWR for freediving in greater depth in a coming issue. Some freediving aficionados say it’s time for a “shift in mindset” on the subject.

Dive Tables Anyone?
Is there a place for dive tables in freediving, similar to those used in scuba? Or for safe IWR?
Dive tables are an amazing tool developed for scuba divers to help prevent DCS, but scuba and tech divers can stop for a while at depth with enough breathing gas to off-gas safely. Freedivers simply don’t have these options and, therefore, it’s just not possible to create the same sort of dive tables for freedivers. However, there are guidelines in place freedivers should follow in order to avoid Taravana. The AIDA 4 manual tell freedivers to either:
- Calculate surface intervals using time by doubling the dive time. For example, if your dive was two minutes long, your surface interval should be at least four minutes long.
Or:
- Calculate surface intervals using depth by dividing the depth in meters by five. For example, a dive to 30 meters should be followed by a surface interval time of six minutes.
AIDA suggests figuring out both calculations and using the most conservative option.
The AIDA guidelines also suggest that, after divers deeper than 55 m/181 ft, divers should abstain from diving for 24 hours and conduct shallow, short warm-up dives beforehand. AIDA has not stated that the agency approves of any sort of IWR or use of O2 after freediving to avoid or treat symptoms of Taravana.
There are whispers of an app that will become available soon to help freedivers to plan their dives and stay safe from Taravana. Watch this space.
Note however there are a number of well established treatment tables for IWR. Here is an example published in the early 1990s in aquaCORPS Journal.

“Australian In-Water Recompression Treatment from “In-Water Oxygen Recompression: A Potential Field Treatment Option for Technical Divers, aquaCORPS # 5 BENT, JAN93. Graph by Richard L. Pyle”
This could be within the realm of possibility in freediving’s distant future. Dr. Valdivia explained that, as of right now, he cannot recommend any form of IWR to freedivers due to lack of research on the subject. He stressed that, “In-water recompression has been done in recent years in freediving; I’ve seen it done with remarkable success in remote locations. But if one wishes to do so, at your own risk, against the position of the freediving agencies, it must be done in very controlled and safe circumstances. It’s a tool that can be successful, but it is an extremely risky tool as well if it is not done properly and safely.”
However, he believes there could be a place for IWR one day. “I hope that there will be more research done in order to standardize such a tool in the future to make it safer,” he said. “If one would partake in IWR, certain criteria must be followed to try to minimize, albeit not eliminate, risk. For example: the designation of roles such as time keeper, coordinator, rotating safeties, and medic; inclusion only of a freediving victim that is awake, alert, and oriented in person, time, place, and situation; a freediver victim that is able to verbalize consent, follow commands, hold on the line, and respond to questions. A full face mask is also mandatory if this takes place. Assessment of conditions such as current, visibility, and temperature/exposure is crucial. There are so many variables that can change that IWR is seldom able to be a controlled situation”.

It could be the case that after much more research, we have enough information to put together a standardized guide or table to follow in order to recompress and alleviate Taravana without (or at least before) the need of a hyperbaric chamber—which is sometimes very far away from the dive location. If we can develop a tool that enables freedivers to be treated for DCS immediately, right there at the dive spot, and in a safe and proper way (approved by medical experts), this could revolutionize freediving safety and potentially save many lives.
It’s clear that much more research needs to be done before we see any official IWR tables in the near future, and more studies on DCS in freediving are needed on the whole. But we are seeing new, record depths every year with no sign of peaking any time soon; with this comes more and more cases of Taravana in the freediving community. But with the expertise of the tech diving community and scientists in the field, we are seeing progress towards making IWR a safer and potentially viable option for freedivers experiencing DCS.
Special thanks to: Dr. Juani Valdivia, Dr. Costantino Balestra, Gary MrGrath, and Marta Marrocco for their help on this article.
DIVE DEEPER
InDEPTH: Do Freedivers Get Bent? By Reilly Fogarty
Alert Diver: Freediving Not a Free Pass Out of DCS
InDEPTH: Is Freediving Safe? By Ted Harty
Scubaboard: Getting Bent Shallow Freedives
Diving and Hyperbaric medicine: In-water recompression by DJ Doolette and SJ Mitchell
InDEPTH: A New Look at In-Water Recompression (IWR) by Reilly Fogarty
Alert Diver: The New Pointy End of Diving by Michael Menduno

For a primer on “technical freediving,” i.e. the use of nitrox mixes to improve safety & performance on breathhold dives, and its origins see: “Technical Freediving: Are Breathhold Divers Ready To Mix It Up?” by Michael Menduno (2019).

Charly is a writer who’s originally from the UK but has been based in Dahab, Egypt, for the past four years. She taught scuba diving for three years in Cyprus, Thailand, and Egypt before discovering her love of freediving. She still scuba dives for fun but, these days, she’s more focused on her freediving training. When she’s not in the water, diving, she’s on her laptop, writing about diving.